Coronavirus overshadows another dangerous viral outbreak

- Share via
SINGAPORE — The first of Yuli Irma’s children to fall ill with a fever was her 6-year-old girl. The next day it was her 13-year-old daughter, followed by her 12-year-old son.
Living on the outskirts of Jakarta, the Indonesian capital, Irma feared her children were stricken with the coronavirus. But blood tests revealed they had dengue fever, another viral disease that’s in the throes of an outbreak but has been overshadowed by COVID-19.
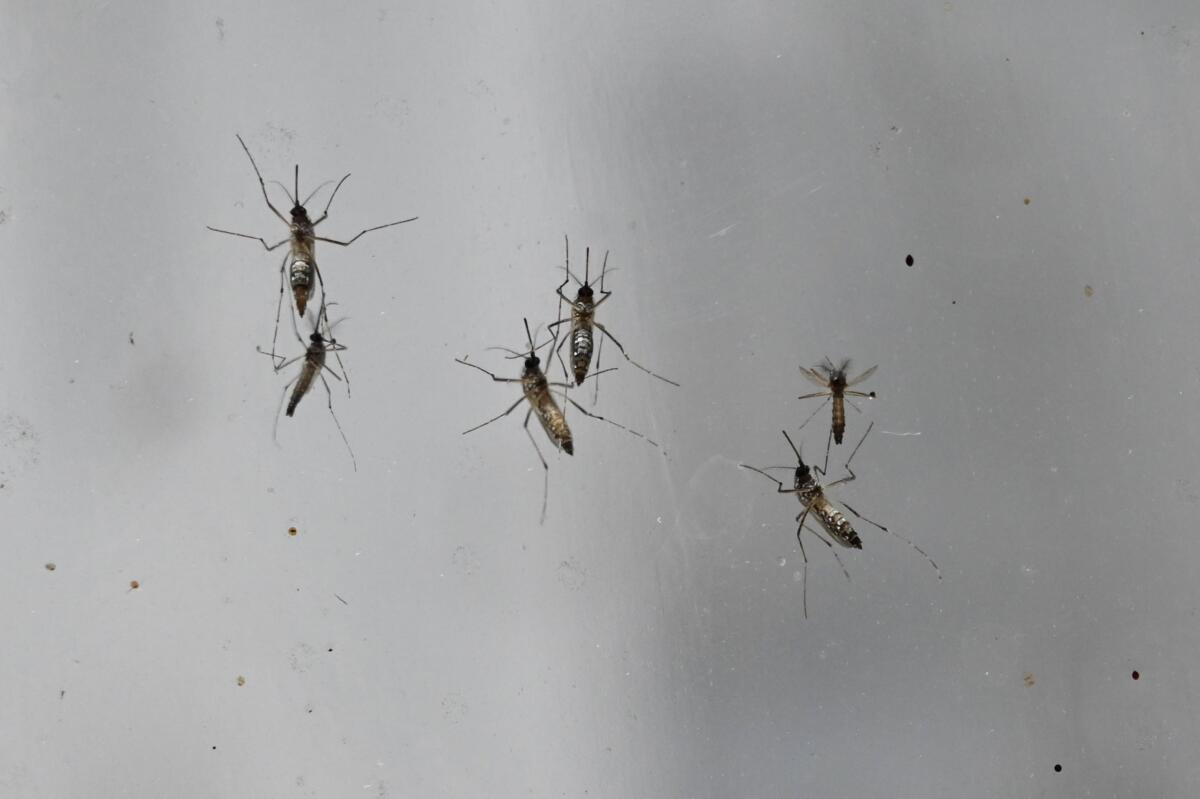
After a record number of cases last year, the illness is relentlessly spreading across Southeast Asia, a hot zone where the mosquitoes that transmit the virus flourish. The painful disease kills thousands each year and infects hundreds of millions within a band of tropical territory spanning the globe.
While the overwhelming majority of people infected never present symptoms, severe cases can result in bleeding, respiratory distress and organ failure. More common symptoms — a few that mirror the coronavirus — include high fevers, severe headaches and excruciating joint pain deserving of dengue’s sobriquet, “breakbone fever.”
The rise in dengue fever cases is further straining medical resources in countries like Indonesia at a time when healthcare facilities are dealing with the crushing demands of a pandemic — a stark reminder of how the coronavirus’ impact on health is rippling far beyond just those it sickens.
People worldwide are delaying elective surgery. Non-coronavirus patients are competing for diminishing supplies of ventilators, antiviral drugs and sedatives. And countries with chronically low numbers of medical staff are being pushed to the brink.
It took days for Irma to find treatment for her children. A doctor drew blood samples at home because Irma feared exposing the youngsters to the coronavirus at a hospital. When the tests revealed dengue, it took several more days to find a facility that wasn’t designated for COVID-19 patients.
“The children were very weak and dizzy by then,” said Irma, 42, whose children were hospitalized for four days in April.

Dengue’s early flu-like symptoms can be confused for the coronavirus. Some patients have been found to have both, exponentially worsening their chances of recovery. The first person with COVID-19 to die in Thailand was also infected by dengue (pronounced deng-ee). In February, two Singaporeans with COVID-19 were misdiagnosed as having dengue.
Like the coronavirus, there is no cure for the disease, though researchers have been trying for decades to develop a vaccine — a sobering prospect for those expecting a COVID-19 vaccine to be ready in less than two years.
Development has been complicated by the fact the dengue virus appears in four different forms, known as serotypes. Patients who recover from one serotype can develop an immunity, but they face severe illness if they’re later infected by another serotyope. A successful vaccine would have to target all four serotypes.
One promising vaccine ended up being marred by controversy. In 2017, the Philippines stopped a vaccination drive that used a drug sold by French pharmaceutical manufacturer Sanofi Pasteur after children began dying.
The government action came after Sanofi Pasteur disclosed its vaccine was making children ill who had never had dengue. The World Health Organization now recommends the drug only for those who have had dengue in the past. The scandal resulted in indictments of government officials and medical researchers in the Philippines, and a public mistrust of inoculations that contributed to a major recurrence of measles last year.
“It’s sort of a cautionary tale while we’re searching for a COVID-19 vaccine,” said Dr. Leong Hoe Nam, an infectious diseases expert at Mount Elizabeth Novena Hospital in Singapore. “Vaccines don’t always behave the way we want them to.”
While dengue is also found in Africa and countries south of the United States, 70% of its occurrence is in Asia. Before 1970, only nine countries had severe dengue epidemics, according to the World Health Organization.
Since then, mass urbanization, explosive growth in travel and warming weather has propelled the spread of the disease, making it endemic in 128 countries. Dengue is considered a “neglected tropical disease,” a title given by health officials to describe illnesses that occur in mostly poorer countries that receive inadequate attention.
The World Health Organization last year named dengue one of the top 10 public health threats and urged countries to improve surveillance of female Aedes mosquitoes, the pests most responsible for spreading the disease (Los Angeles County experienced an outbreak of Aedes mosquitoes as recently as 2018).

Experts are unsure what impact social restrictions and widespread lockdowns will have on the spread of the disease. Aedes mosquito bites most commonly occur inside homes, which is where people are now confined.
The likelihood of infection “is probably increased with everyone staying at home, but the lack of mobility may limit its spread,” said Duane Gubler, founding director of the Emerging Infectious Diseases Signature Research Program at Duke-NUS Medical School in Singapore. “We’re going to have to wait and see.”
Dengue outbreaks tend to come in waves lasting several years. The duration of outbreaks depend on populations developing herd immunity to strains of the virus before a new one can gain momentum.
Countries such as Singapore have learned to live with the disease by promoting what amounts to social distancing with mosquitoes.
Citizens here are regularly reminded by inspectors to eliminate sources of stagnant water. Construction sites, prime places for puddles, must include on-site pest control officers charged with eliminating larvae. And residential neighborhoods are periodically doused with plumes of organic insecticides, a practice known as fogging.
Earlier this month, the country’s National Environment Agency expanded a program releasing male mosquitoes loaded with bacterium designed to prevent eggs from hatching after mating.
Despite increased vigilance, however, dengue cases, including a senior member of Parliament, have doubled compared with the same period last year, to 6,900 — all while the country’s health network has had to treat nearly 25,000 coronavirus patients.
“We are all susceptible to dengue and it’s a war we can’t fight alone. We need each other, more than ever before,” Low Yen Ling, a member of Parliament since 2015, wrote on her Facebook page.
Guo Xian has been vigilant since he saw public health banners up in his central Singapore neighborhood warning of a local dengue outbreak. The radio producer contracted the disease three years ago and had to be hospitalized with a high fever and a rash. To reduce his chances of getting dengue again — and facing an even worse episode — he has reduced his morning jogs and begun applying mosquito repellent liberally, even indoors.
“Ever since I got discharged, I’ve been paranoid,” said Guo, 46, who feels dengue sapped him of some of his energy. “You’ve always got to be careful, especially now because of dengue and COVID-19.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.