How dexamethasone might lead researchers to better COVID-19 treatments
- Share via
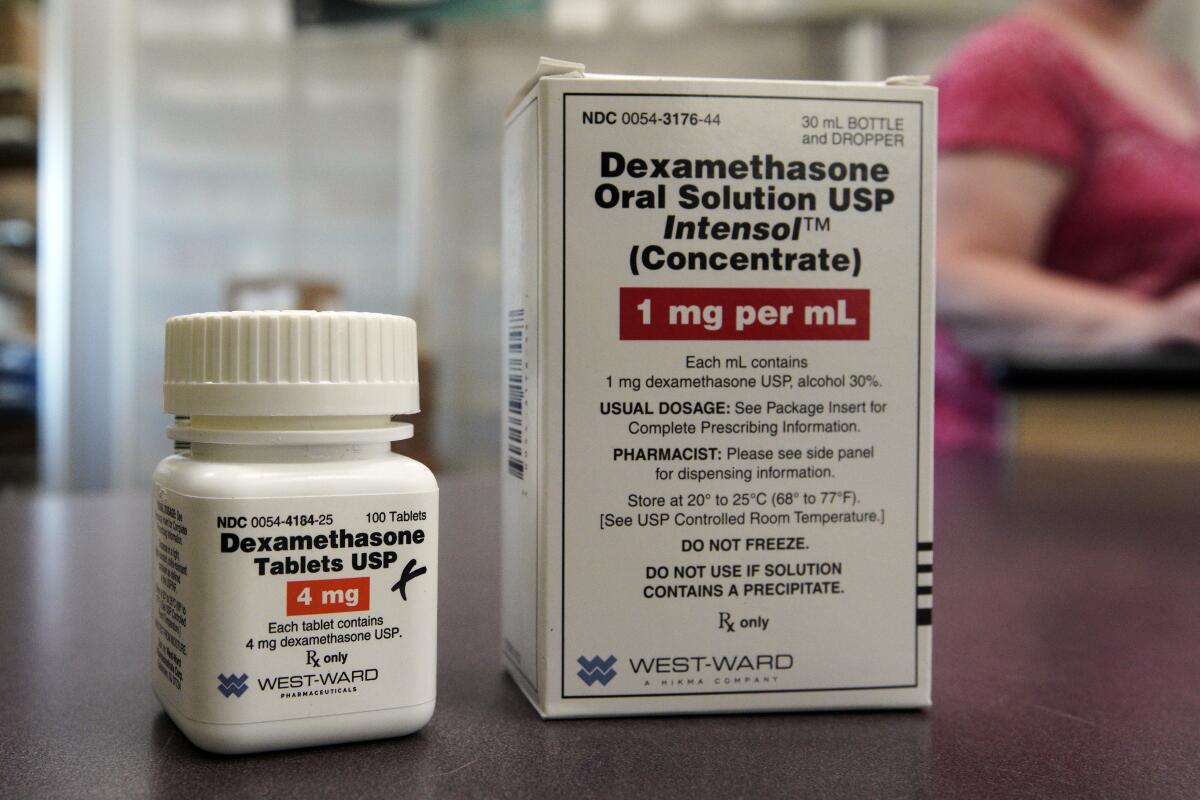
New evidence that a common corticosteroid drug can be lifesaving for those with severe COVID-19 has set off deeper debates about what goes wrong with COVID-19 and how best to fix it.
In preliminary clinical trial results announced Tuesday, patients on mechanical ventilators who were treated with the steroid dexamethasone were 35% less likely to die of COVID-19 than their counterparts who got standard care without the drug. And in patients whose illnesses were slightly less severe — requiring supplemental oxygen but not breathing machines — a 10-day course of low-dose dexamethasone reduced mortality by 20%.
Critical-care physicians are assessing the findings and considering whether the treatment is appropriate for their patients.
Scientists, too, are poring over the fine print of the British trial’s design, doses, and data to see what they might reveal about the “how” of dexamethasone and the coronavirus itself.
The steroid medication is widely thought to suppress the abnormal — and dangerous — inflammatory responses in some patients with severe COVID-19. But by what precise mechanism it does so is unclear.
Researchers in England say drug can reduce death rates in very ill COVID-19 patients. But it’s risky for those with mild symptoms.
Unraveling this mystery won’t be easy, considering the complexity of the immune system and its multiple layers of defense.
Dexamethasone acts indiscriminately on several distinct types of so-called interleukin proteins that are involved in regulating the body’s immune response. The steroid suppresses their activity by shutting them down close to their source in white blood cells.
If scientists could narrow down which of those proteins most effectively reduces mortality risk in COVID-19, they might be able to quell the most damaging inflammation and leave other, potentially helpful immune system processes undisturbed.
Sometimes called a “cytokine storm,” the blast of inflammation that afflicts a small percentage of COVID-19 patients can cause serious damage to lungs. It also appears to scar and damage small blood vessels and the many organs that rely heavily on such microvasculature, including the brain and kidneys.
But where and how dexamethasone counters such damage was not clear from the British trial results.
A medication like dexamethasone is a “blunt instrument,” said Dr. Steven J. O’Day, who directs the John Wayne Cancer Center at Providence St. John’s Health Center in Santa Monica. It’s not clear where, exactly, the steroid is having its positive effect for patients with widespread inflammation. Nor is it clear where tamping down inflammation matters most in rescuing a patient from death.
“This study is not telling us if this drug is even acting on the lungs,” said Dr. Craig Coopersmith, who directs Emory University’s critical care center and routinely cares for COVID-19 patients. “There could be a host of scientific reasons” it’s working, he added.
Scientists will need to conduct more research on dexamethasone to answer questions like these and tailor treatments to patients with differing mixes of symptoms, Coopersmith said.
COVID-19 has killed more than 100,000 people in the U.S., but some are more vulnerable than others. These charts show how Americans have been affected.
Part of that challenge will be to discern which feature of COVID-19 is deadliest.
The final stage of the disease most closely resembles one of two critical illnesses often treated in hospital intensive care units. To some doctors, it looks and acts most like septic shock, in which several organs progressively fail. To others, it behaves most like a lung affliction — acute respiratory distress syndrome, or ARDS — that can be caused by injury, chronic diseases like emphysema, or infections such as flu and bacterial pneumonia.
While steroid medications like dexamethasone are widely used to treat septic shock, they are not viewed as safe and effective for treating ARDS.
There’s another condition that looks remarkably similar to severe COVID-19, O’Day said: the side effects suffered by some cancer patients taking immunotherapy.
In those patients, cytokine storms tend to clear quickly when treated with targeted medications usually used for patients with rheumatoid arthritis.
Two such medications, tocilizumab (marketed as Actemra) and sarilumab (Kevzara), are also being investigated in clinical trials as treatments for COVID-19. While they would be far more expensive than dexamethasone, they may prove to more specifically target the processes that cause greatest harm in COVID-19, O’Day said.









