New method for predicting breast cancer risk suggests about 30% of cases could be prevented
- Share via
Ask almost any health-conscious woman who’s mustered under a giant pink ribbon, and she’ll tell you what an American woman’s chances are of getting breast cancer in her lifetime: 1 in 8.
But that’s a national average. And as the relative influence of genes, behavior and environmental factors on cancer risk come into clearer focus, women increasingly have begun to understand that they’re not all average.
New research is helping to refine those numbers, and to clarify what it would take for a woman to reduce her risk of developing breast cancer. It concludes that, at some point in her life span, a 30-year-old white woman in the United States has a probability of developing breast cancer that lies somewhere between 4.4% and 23.5%.
Published Thursday in the journal JAMA Oncology, the study concludes that as many as 29% of breast cancer diagnoses among such women could be prevented or delayed if all women maintained a healthy body weight, did not use menopausal hormone therapy, drank little and did not smoke.
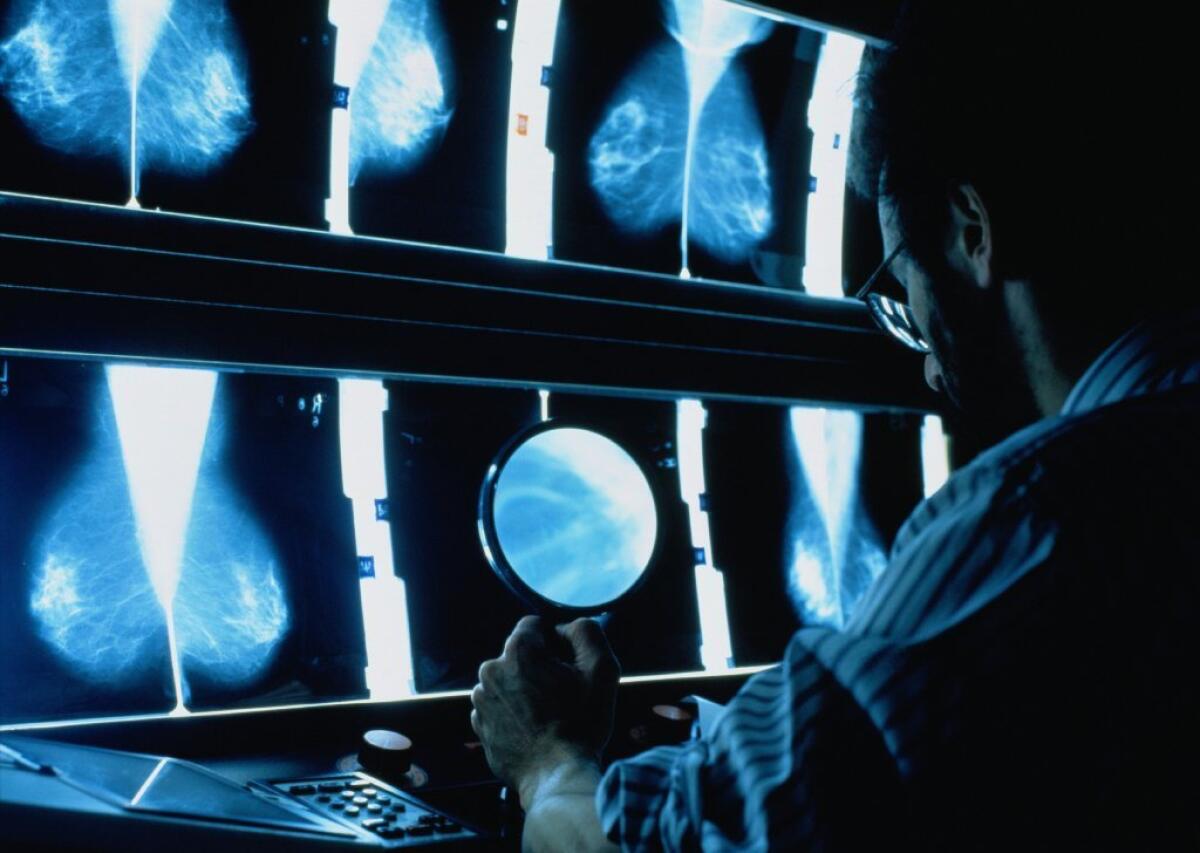
The question of whether breast cancer can be prevented, in whom and by how much is as important as it is murky. Against a backdrop of uncertainty and dispute among experts, a woman nowadays needs to decide how early and how often she should get a mammogram, whether she should take a pass on hormonal therapy, or whether taking a medication to reduce her breast cancer risk might be worth the possible side effects.
To make good decisions, she needs a better, more personalized gauge of her chances of developing breast cancer. And sometimes she needs motivation to make healthy behavior changes -- especially if she is an overweight woman or one who smokes or drinks alcohol.
Until now, there have been the standard breast-cancer prediction models: the one in widest use is called the Gail model. These risk calculators generally ask a woman’s age, about breast cancer in her family, when she started menstruating, how many pregnancies she’s had and when, and whether she’s ever had an abnormal finding on a mammogram or a breast biopsy. If a family history sends up red flags, genetic testing that looks for two well-known gene mutations -- BRCA1 and BRCA2, which can boost as much as fivefold a woman’s breast cancer risk -- might be recommended.
Beyond factors like those, things get fuzzy. A physician might mention alcohol consumption and obesity as factors to consider. But the role of these “modifiable factors” — health behaviors a woman can actually do something about — has not generally been cranked into existing prediction models. Nor do those models consider the role of at least 92 genetic variations that appear to influence breast cancer risk, but far less powerfully than do the BRCA1 and BRCA2 mutations.
The new research, led by epidemiologists and biostatisticians at Johns Hopkins University and the National Cancer Institute, sets out to change that. It finds that those women who are at greatest risk of developing breast cancer due to factors beyond their control, are the same women who most steeply reduce their risk when they maintain a healthy weight, stay away from hormone replacement therapy, don’t smoke and drink little to no alcohol.
To glean such findings, the team combed through eight studies that followed large numbers of women for several years and reliably captured all cases of breast cancer diagnosed among participants. On the basis of some 37,000 mostly white women in the United States, Europe and Australia, they built a model of risk across the population. Then, they projected those findings on the population of white women in the United States.
To calculate the risk that participants faced from fixed factors — things like genes they could do nothing to change — the researchers combed the women’s genetic information in search of 24 single nucleotide polymorphisms, or SNPs, that have been loosely linked to breast cancer. For another 68 SNPs that have been identified as breast-cancer-related but far less studied, the authors extrapolated from other study findings on how often they would occur and how powerfully they would drive breast cancer.
They then added that information to data already used to compute breast cancer risk: factors such as onset of menstruation, pregnancy and age.
The approach, said medical oncologist Dr. Rachel Jankowitz, is a unique twist on existing risk prediction models: First, it ascertains how high (or low) a woman’s breast cancer risk is on the basis of factors she can’t do anything about; then, she said, it asks how much (or little) the factors she can control could affect that risk.
“This has great potential. It’s what we’ve been waiting for — a way to counsel women specifically,” said Jankowitz, who practices and conducts research at University of Pittsburgh’s Cancer Institute and was not involved in the study. “It’s not ready for prime time but boy, could we use something like this.”
See more of our top stories on Facebook >>
Follow me on Twitter @LATMelissaHealy and “like” Los Angeles Times Science & Health on Facebook.
MORE IN SCIENCE
Antidepressants aren’t just for depression anymore, study finds
Can treating the brain help in the fight against diabetes?
In politics, it’s not what you say but how you say it, acoustical analysis shows




