Coronavirus Today: The true danger of Omicron
Good evening. Iâm Karen Kaplan, and itâs Tuesday, Aug. 16. Hereâs the latest on whatâs happening with the coronavirus in California and beyond.
Back in December, when South Africa was taking stock of the worldâs first COVID-19 surge fueled by the Omicron variant, health experts were pleasantly surprised by what they saw.
In the province of Gauteng, new infections matched the record previously set by Delta â and did so much faster, thanks to Omicronâs unprecedented ability to spread. But the new variant caused much less damage along the way.
The risk of hospitalization among infected adults was 29% lower than in earlier surges, and the chances of being admitted to an ICU were lower as well. Pieter Streicher, a coronavirus analyst at the University of Johannesburg, projected that hospitalizations would wind up being 25 times lower than would normally be expected for such a high infection rate.
Even better: Across the country, the death rate among people who caught the coronavirus fell precipitously during that initial Omicron wave.
Observations like these were repeated around the world as Omicron crossed borders and oceans with shocking efficiency. It didnât take long for Omicron to gain a reputation for being a kindler, gentler version of SARS-CoV-2.
Now, as policymakers and regular folks wonder whether itâs time to stop disrupting our lives for the sake of avoiding infection, some scientists are pointing out an inconvenient truth: We still donât actually know whether Omicron is actually more mild than its predecessors.
We do know that Omicron has caused less damage. But that could say more about the conditions in place when Omicron arrived on the scene than the intrinsic properties of the virus itself.
âItâs widely said that Omicron is inherently less pathogenic, but there is no real evidence for that,â Dr. Christopher Chiu, a COVID-19 researcher at Imperial College London, told my colleague Melissa Healy.
By the time Omicron reached U.S. shores just after Thanksgiving, Americans had a substantial level of immunity. Sixty percent of us had been fully vaccinated, and roughly a third had immunity from a past infection. (Those groups overlapped, though by how much isnât clear.)
Plus, those who became infected anyway had the benefit of treatments that werenât available during earlier surges caused by the original strain from Wuhan or the Alpha and Delta variants it spawned.
If Delta had arrived under those conditions, perhaps it would have seemed mild too.
âComparisons with Delta are like apples and oranges,â Chiu said. âDelta was circulating at a time when many were still not vaccinated or previously infected. In contrast, Omicron is largely causing breakthrough infections in people who already have partial protection from immunity conferred by vaccines or infection.â
Trying to determine how much of Omicronâs benevolence is due to its inherent characteristics isnât easy. One study published in the journal Nature found that in petri dishes, Omicron attacked cells of the upper respiratory system with less gusto than Delta. Omicron was also much less adept at infecting lung tissue and other cells in the lower airway.
Other studies conducted in animals such as hamsters and mice found that critters infected with Omicron lost less weight than those infected with Delta. Thatâs telling because the more serious an infection, the more weight is lost. The animal studies also showed that Omicron triggered less inflammation in the lungs.
An ideal way to find out whether Omicron is intrinsically less dangerous would be to round up people whoâve had the same number of vaccine doses and past infections, then deliberately infect them with different versions of the virus and see how they fare.
If that kind of study sounds familiar, itâs because Chiu has conducted one like it in London to see what the original coronavirus strain does to the body. Now heâs working up plans for a follow-up trial that would use Delta and Omicron. The results could provide a clearer picture of whether Omicron goes easier on its victims.
The answer really matters. If if it turns out that Omicronâs reputation for treading lightly is warranted, we can dial back our pandemic precautions with confidence. On the other hand, if Omicron is just as virulent as its predecessors, we may need to keep our guard up a little longer.
âItâs an excellent question,â said Dr. Stanley Perlman, a University of Iowa virologist and a leading expert on coronaviruses. The true picture is ânot clear.â
By the numbers
California cases and deaths as of 2:50 p.m. on Tuesday:
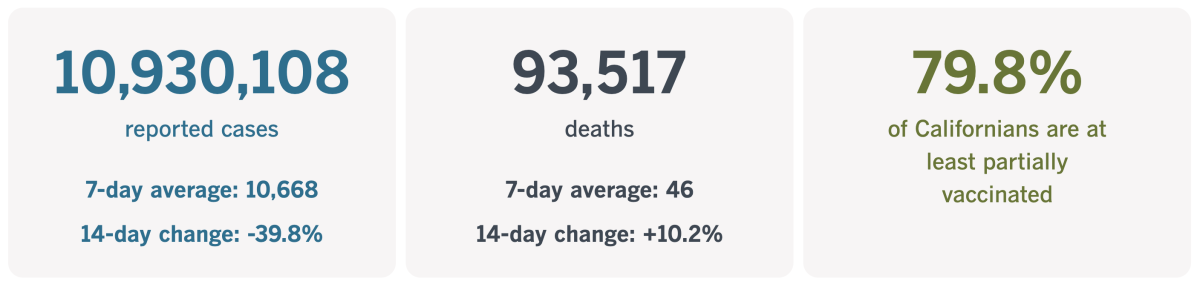
Track Californiaâs coronavirus spread and vaccination efforts â including the latest numbers and how they break down â with our graphics.
What it takes to remain a coronavirus virgin
My colleague Gustavo Arellano wears a lot of hats. Heâs the host of The Times, our daily podcast about news and culture. Heâs a regular columnist for the California section. He pinch-hits with writing the Essential California newsletter.
Apparently that wasnât enough to keep himself fully occupied. He recently called Los Angeles County Public Health Director Barbara Ferrer to volunteer his services for another assignment: COVID-19 success story.
Arellano is part of the dwindling minority of Americans who are still coronavirus virgins. Not only has he avoided the hyper-contagious Omicron variant and its assorted subvariants, to the best of his knowledge he hasnât been infected with any version of the coronavirus since the pandemic began.
âI thought I was special, someone worthy of a case study,â Arellano wrote.
Itâs unclear how big this group is. But with the United States averaging roughly 95,000 new infections over the last week, itâs safe to say that the ranks of the never-infected are getting smaller by the day.
A report led by researchers on the Centers for Disease Control and Preventionâs COVID-19 Response Team estimated that 58% of U.S. residents had been infected at least once by February. That figure was based on an ongoing study that screens blood samples sent to clinical laboratories to see if they contain antibodies that are produced only in response to a coronavirus infection. (Specimens from people with suspected cases of COVID-19 are excluded from the analysis so they donât skew the results.)
By mid-July, near the peak of the BA.5 surge, the percentage of Americans whoâve had at least one coronavirus infection had climbed all the way to 82%, according to models developed at the Institute for Health Metrics and Evaluation at the University of Washington.
Arellano has seen the number of the never-infecteds shrink in his own social circles. Among those closest to him, heâs now the only one left with no firsthand experience with the virus. (This despite the fact that theyâre all fully vaccinated and double-boosted.)
That counts as an accomplishment in my book. But in Ferrerâs professional opinion, it didnât make Arellano enough of an anomaly to warrant turning him into some kind of case study.
âIâm not really that surprised,â she told Arellano after hearing about his status. âThereâs still a couple of million people in L.A. County who havenât contracted it yet.â
Ferrerâs assessment was that Arellano benefitted from good luck and perhaps also some good genes. But the main thing working in his favor was that he exercised caution â especially by wearing a mask.
âWeâve been in such a fight about the mask, but most of the people who have told me they havenât received COVID tell me theyâve been wearing a mask,â Ferrer said.
Arellano admitted that he resisted masks at first. Heâd wear one for work assignments but not when he was off the clock.
âI found them silly and felt self-conscious wearing one â highlighted my big forehead, you know?â he said. When he did cover up, he opted for a bandana.
It was his wife, Delilah Snell, who persuaded him to change his ways. Thanks to her prodding, Arellano graduated to a cloth mask, then a surgical one, then to a high-quality N95 âthat I now wear as comfortably as a windbreaker,â he said.

Snell is the proprietor of Alta Baja Market in Santa Ana. Arellano has written that patrons of the cheery shop and bistro are required to wear masks unless theyâre sitting down and eating.
The message is hard to miss â last summer, as the Delta variant was surging, no fewer than five signs about the mask policy were posted to the marketâs front doors. Customers who donât have a mask of their own are invited to take one from a basket near the entrance.
There were no exceptions for spouses.
âWhat converted me was my wife telling me Iâd be banned from her store if I didnât wise up,â Arellano wrote.
That vigilance has paid off: Snell is also a coronavirus virgin.
In her view, thereâs nothing complicated about it â no reason why scientists would want to study either her or her husband.
âWear a mask!â Snell interjected as Arellano was speaking with Ferrer. âThis pandemic wouldâve been over long ago if people just wore their masks!â
Ferrer appreciated the remark.
âYour wife has been right from the very beginning,â she said. âListen to her more. She has the wisdom of women taking care of each other.â
Californiaâs vaccination progress
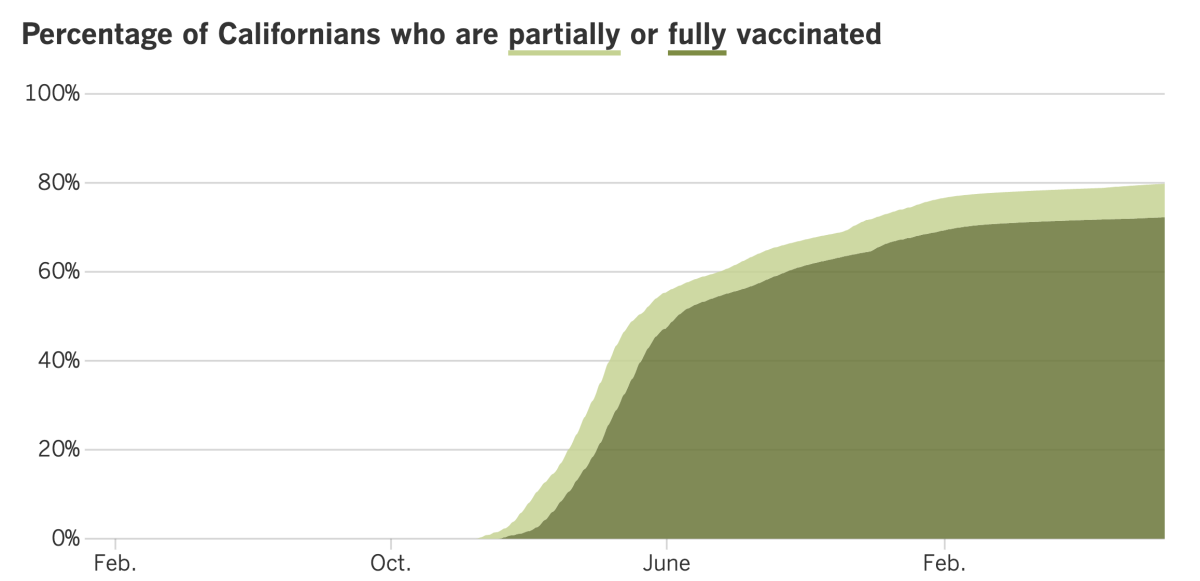
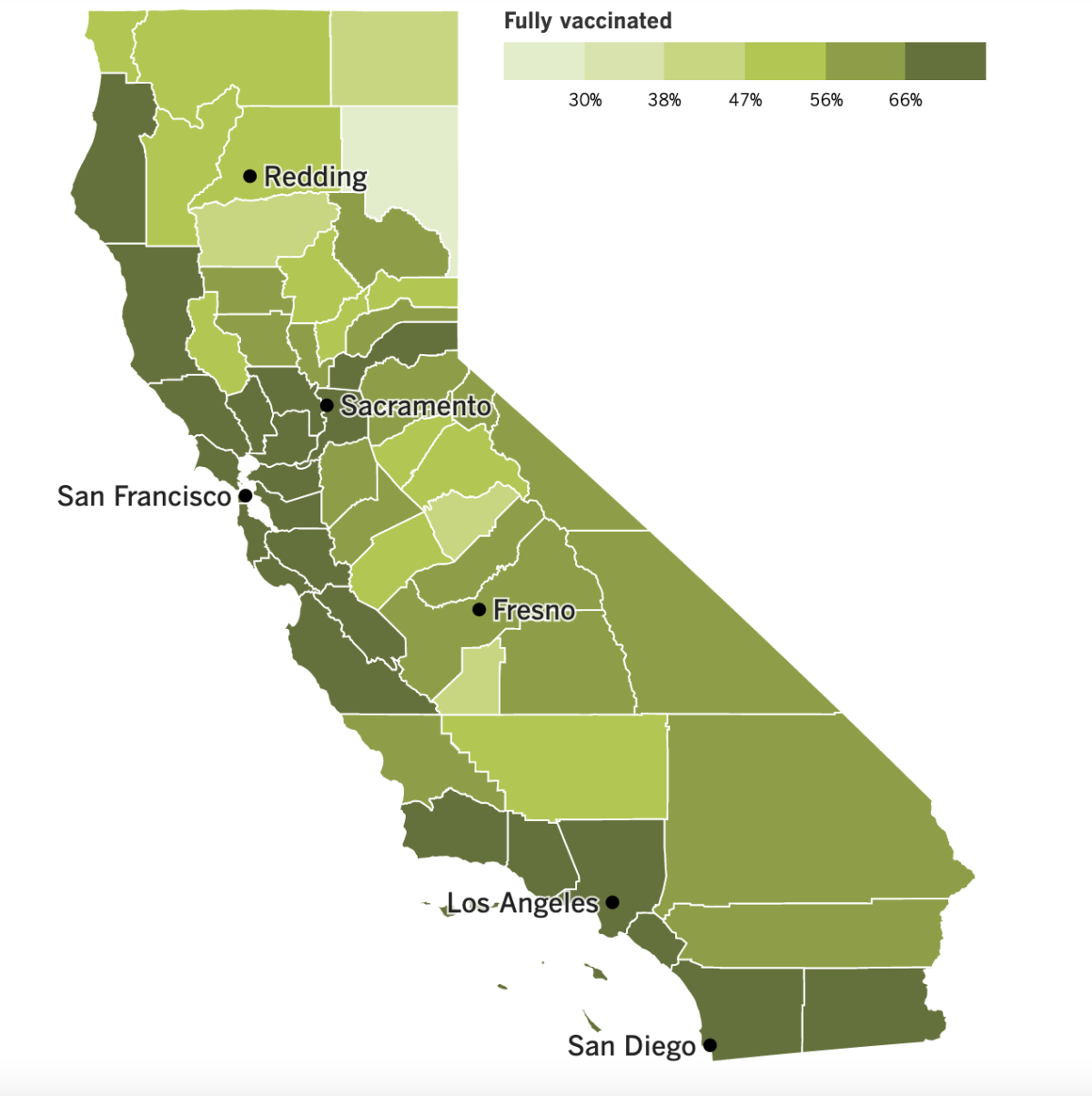
See the latest on Californiaâs vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Congratulations, Los Angeles County! Youâve officially downgraded your COVID-19 community level.
The latest assessment from the CDC knocked L.A. out of the âhighâ category and into âmedium.â The federal agency said Thursday that the countyâs coronavirus case rate over the prior week was nearly 302 per 100,000 people, which is considered high. But the number of newly hospitalized patients with coronavirus infections over the prior week dropped from 10.1 to 9.9 per 100,000 people, according to the CDC. Falling below 10 was the key for moving from âhighâ to âmediumâ territory.
County health officials unofficially moved themselves out of the âhighâ category back on July 28. On that date, the CDC said L.A. had 10.7 newly hospitalized coronavirus-positive patients per 100,000 residents over the prior week. But Ferrer said that based on her departmentâs more up-to-date figures, the actual number was 9.7. (That statistic spared the county from a new indoor mask mandate.)
According to a Times analysis of county data, the average number of reported new infections per day fell 23% week to week, to just 263 new cases per 100,000 residents per week. Thatâs better than 302 per 100,000 people but still considered high.
âBecause viral transmission remains high, there are still thousands of new people each day who are infected and therefore capable of infecting others,â Ferrer said.
And yet everywhere you look, it seems that more and more people are ready to set aside their infection-prevention routines. The CDC is trying to keep them in the game with new guidelines that streamline its most recent advice.
Very little is different in the new guidelines. Getting vaccinated and boosted as soon as youâre eligible remains at the top of the list, as does the recommendation to get tested if you suspect you may be infected. However, widespread testing to screen large populations of asymptomatic people is now recommended only for those in high-risk settings, such as nursing homes and prisons. The same goes for contact tracing (though such efforts have already been scaled back.)
Those who test positive are still urged to isolate for at least five full days and to exit isolation only after their COVID-19 symptoms have improved and they have been fever-free without taking medicine for at least 24 hours. The agency is sticking to its disputed stance that a negative coronavirus test is not required to end isolation.
But it now says thereâs a role for testing if people donât want to keep wearing a mask until the end of their 10th day: If you test negative on Day 6 or later, then test negative again 48 hours after that, you are free to ditch your mask, according to the CDC.
Some people should plan to isolate for at least 10 full days, including those who experienced shortness of breath or other breathing problems, patients who required treatment in a hospital and people who are immunocompromised. But the new guidelines deemphasize the need to quarantine if youâve been exposed to someone whoâs infected but havenât tested positive yourself. Instead, you should wear a high-quality mask when youâre around others (in case you do end up with an infection) and test yourself at least five days after exposure to to see if youâre infected.
The Food and Drug Administration is out with some new advice of its own regarding coronavirus tests. Instead of taking two rapid antigen tests to make sure youâre not infected, the FDA now says youâll need three. The change is based in part on the results of a government study that found that adding a third test to the regimen significantly improved the accuracy of the results.
Drug regulators in the U.K. have become the first in the world to authorize a new version of Modernaâs COVID-19 vaccine that targets the Omicron variant in addition to the original coronavirus strain. The combination vaccine will be offered to people 50 and older as a booster shot, according to the Medicines and Healthcare Regulatory Agency.
Moderna and Pfizer are working on similar âbivalentâ COVID-19 vaccines for the U.S. market. But the U.K. vaccine is a little different: The version of Omicron itâs designed to recognize is BA.1, while the vaccines being readied for the U.S. will go after the BA.4 and BA.5 subvariants. The most recent estimates from the CDC are that those two strains account for more than 94% of the SARS-CoV-2 coronaviruses in circulation here.
And finally, this weekâs list of celebrity COVID-19 patients includes First Lady Jill Biden (who has mild symptoms), Defense Secretary Lloyd J. Austin III (who already had COVID-19 during the first Omicron surge in January) and Pfizer Chief Executive Albert Bourla (who has received four doses of his companyâs Comirnaty vaccine and is now taking its Paxlovid antiviral pill).
Your questions answered
Todayâs question comes from readers who want to know: How can my child avoid COVID-19 at school?
Whether your child is starting kindergarten or embarking on the last year of high school, the simple act of spending hours inside classrooms with dozens of other students is bound to lead to coronavirus exposure at some point. (One of my sonâs classmates brought the virus with him on the very first day of school.)
But exposure doesnât have to lead to infection, and the American Academy of Pediatrics has this advice for keeping children safe:
⢠Make sure your student is vaccinated against COVID-19. Being up to date on vaccinations is âthe single most effective way to protect children,â said Dr. Sonja OâLeary, who chairs the academyâs Council on School Health. Everyone who is at least 6 months old is eligible for a COVID-19 vaccine, and kids 5 and up may be eligible for a booster.
⢠Consider wearing a mask while indoors at school. Even if itâs not required, itâs still helpful â especially for students who are unvaccinated, immunocompromised, have a family member at high-risk of becoming severely ill, or live in a county with a high COVID-19 community level. A mask that fits well around the nose and mouth is best.
⢠Remind students to wash their hands frequently and thoroughly. This is particularly important before eating.
⢠Keep kids at home if they are sick.
If sending your child back to school makes you a little nervous, you may be comforted to hear that the academy says the risks are manageable and worth taking.
âOne of the most critical lessons of the pandemic was that children are more likely to learn, thrive and develop appropriately when attending school in-person alongside their peers,â AAP said in a statement.
We want to hear from you. Email us your coronavirus questions, and weâll do our best to answer them. Wondering if your questionâs already been answered? Check out our archive here.
The pandemic in pictures

Backpack? Check.
Water bottle? Check.
Face mask? Check.
The students in the photo above â 5-year-old Isabella Sosa and her 4-year-old brother Daniel Sosa â opted to start their new school year at Vena Avenue Elementary in Arleta with colorful masks on their faces. Itâs just a sign of the times.
The siblings were among the roughly 437,000 students in the Los Angeles Unified School District who kicked off a new school year on Monday.
It was the districtâs third first day of school since the pandemic began. Both parents and educators said they were hopeful that life on campus would feel almost normal this time around.
âIâm excited for my son to learn,â said Donovan Donaldson, a parent at Plummer Elementary in North Hills.
Students were eager too, including Haley Henderson, a junior at King/Drew Magnet High School of Medicine and Science in Willowbrook whoâs still wistful about spending her entire freshman year at home. âIâm really excited to be here,â she said, âso I think that fills that void.â
Resources
Need a vaccine? Hereâs where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Hereâs what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
Weâve answered hundreds of readersâ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




