Racial gaps in healthcare still cost black lives, though Obamacare narrowed them

- Share via
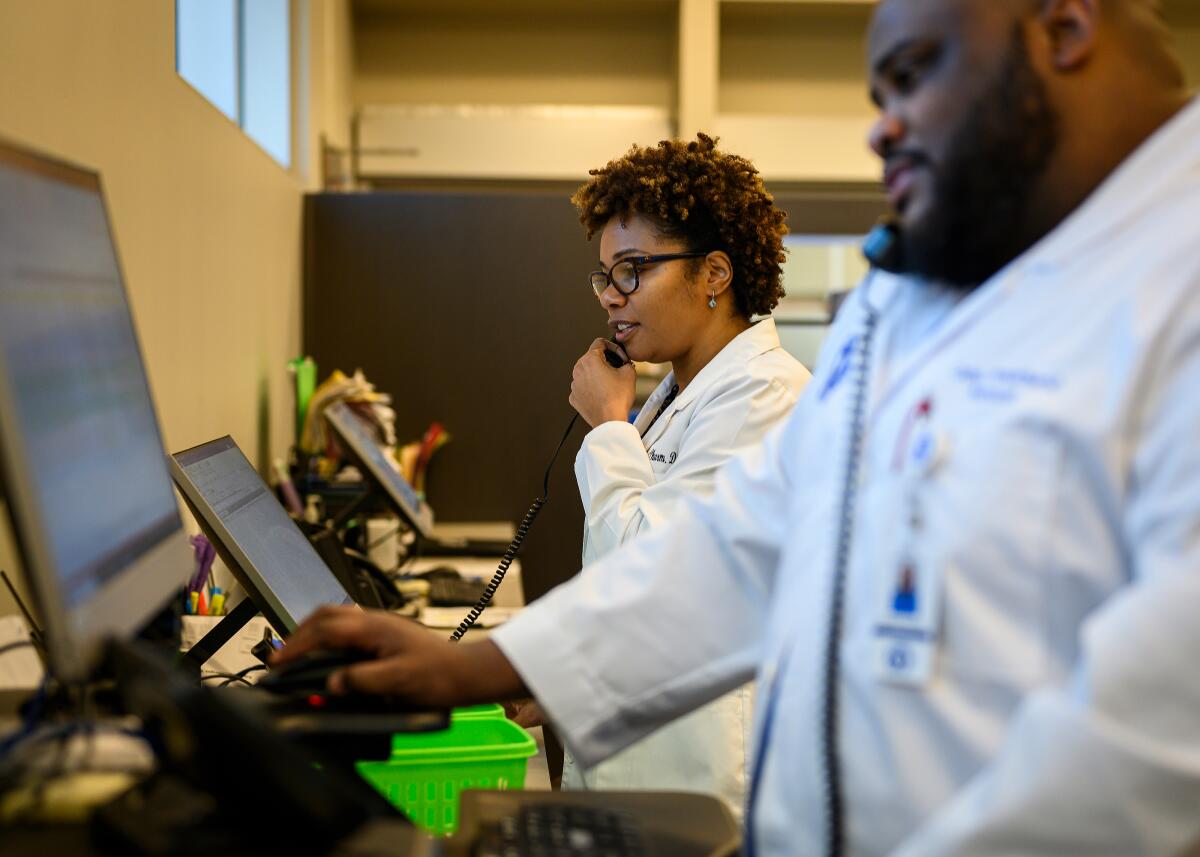
WEST MEMPHIS, Ark. — Dr. Susan Ward-Jones observed something remarkable not long after the East Arkansas Family Health Center opened a new clinic in this small city by the Mississippi River.
“People used to come in unkempt, sloppily dressed. They look better now,” said Ward-Jones, the clinic’s director. “I think people have a new pride in themselves. Maybe they see we’re doing better and they say, ‘I’ll try to do better, too.’”
With a two-story glass atrium and soaring brushed metal portico, the clinic — whose patients are mostly poor and African American — has nearly twice as many exam rooms as the health center’s old location in a cramped storefront down the road. Nine dental suites, a pharmacy and a state-of-the-art demonstration kitchen branch off the sun-dappled atrium. A shaded exercise track winds through a stand of tall oaks out back.
As nationwide protests highlight the continued impact of racism in criminal justice, the struggle to create and maintain health centers like this one — and over the law commonly known as Obamacare — offers a window into the tangled history of race and healthcare in the U.S., as well. The clinic opened in 2014, thanks to the Affordable Care Act, which also helped thousands of its patients get health insurance.

“The Affordable Care Act empowered people who didn’t have power. It’s given people a measure of self-respect. That’s been very profound,” said Dr. David Satcher, the former U.S. surgeon general who grew up in the South when many hospitals didn’t allow black physicians like him to admit patients.
More darkly, the reaction to the law — whose passage in March 2010 was shadowed by racist outbursts from some opponents — also has revealed troubling fault lines that remain.
The 14 states that continue to oppose expansion of Medicaid insurance made possible by the law are concentrated in the South, effectively maintaining large racial disparities in access to care. Most of those same states are suing in federal court to have the law invalidated.
“It may be too simplistic to say that opposition to the Affordable Care Act in the South is just about race,” said Thomas J. Ward Jr., a historian who has written about healthcare and civil rights. “But you can’t look at opposition to expanding health services, and not see that some of that opposition is rooted in race in a significant way — not necessarily straight racial animosity, but fear of racial empowerment.”

Today, a new chapter in this complicated story is being written as the coronavirus outbreak disproportionately affects African American communities across the country, once again spotlighting the racial disparities that shadow American healthcare.
The connection between healthcare and race has been particularly resonant along the Mississippi River, where access to medical care was long a dividing line as rigid as separate schools and drinking fountains, and where federal healthcare initiatives half a century ago helped end segregation.
Clifton Collier, who ran a health center in Marianna, Ark., 50 miles south of West Memphis, lived a good part of this history.
Collier, 66, grew up in the heart of the Arkansas Delta, an expanse of dark, fertile earth stretching over bayous and through thick stands of cedar and live oak along the west bank of the Mississippi.
This was one of the last bastions of the Jim Crow South, a ferociously segregated place where former plantation homes still dot the landscape and a commanding statue of Robert E. Lee on the town square bears testimony to the persistence of the old system.
Collier’s was better off than most black families. His father ran a juke joint that did a brisk business, particularly on Sundays. And just outside town, in a place called Black Swamp, the family owned land it had bought after the Civil War. Some in the family say part of the money came from a white man who fathered one of Collier’s ancestors.
As children in the 1960s, Collier and his siblings worked the cotton fields around Black Swamp, lugging burlap sacks up and down long rows and pulling white bolls from between the plants’ needle-like stems.
If anyone got sick, they’d see a local black woman who practiced folk medicine. “We didn’t have money for a doctor,” Collier recalled. “Nobody did.”
None of the town’s four white doctors would see a black patient who didn’t have cash. “We just had to take care of ourselves,” Collier said.
That didn’t seem to trouble the physicians, who told a CBS News crew that visited Marianna in 1969 that black patients got what they needed. “They get adequate medical care if they come seeking it,” one doctor said. “So many times, they’re sick, and they don’t seek it because of ignorance or laziness.”
Cracks in this system began to emerge following passage of the 1965 law that created Medicare, the government insurance plan for the elderly and disabled. The law barred federal money for segregated institutions, forcing hundreds of hospitals across the South to desegregate waiting rooms, patient floors and nurseries almost overnight.
A second federal initiative helped bring community health centers such as Collier’s clinic to many of the poorest quarters of America, offering reliable medical care to black patients in places like the Arkansas Delta for the first time.
These clinics weren’t universally welcomed. When volunteers tried to open the Lee County Cooperative Clinic in Marianna in 1968, white landlords refused to rent space.
The local medical society blocked the clinic’s first doctor, a young physician from St. Louis, from admitting patients to the hospital in Marianna, forcing them to travel to Memphis or Little Rock, more than an hour away. Several workers at the clinic were beaten up outside a local restaurant.
But the clinic endured. Such health centers were designed to empower the low-income patients they served, with federal money funneled directly to the clinics, bypassing white-controlled state governments. In Lee County, clinic volunteers helped develop a slate of black candidates for local office.
“The clinic turned out to be the opening chapter of the civil rights movement in Lee County,” recalled Dr. Dan Blumenthal, the clinic’s first doctor, who taught at Atlanta’s Morehouse School of Medicine until he died last year.

The health centers — and federal programs such as Medicare and Medicaid — had a profound impact on the lives of black Americans.
Across the Mississippi River from Marianna, a federally funded health center in Mound Bayou, Miss., helped cut the infant mortality rate among African Americans in the surrounding county by more than a third in just four years, researchers found.
Nationwide, access to care also improved dramatically. In 1964, white Americans were nearly 50% more likely than their black counterparts to have seen a doctor in the previous two years. Three decades later, that reversed, with African Americans more likely than whites to have been to a doctor recently.
Nevertheless, by the time President Obama and congressional Democrats began pushing for the Affordable Care Act, substantial racial inequalities in healthcare remained.
Black Americans were more likely to be uninsured, more likely to report financial barriers to getting care and more likely to die from treatable diseases.
Obama didn’t cite these disparities, focusing instead on the promise of guaranteed health coverage for all Americans.
“Race wasn’t the focus,” a former senior Obama aide recalled. “We didn’t go there.”
But race was never far in the background of the debate.
Rush Limbaugh, Glenn Beck and other conservative commentators who vigorously opposed the health law repeatedly claimed it was part of Obama’s strategy to make the federal government compensate African Americans for slavery.
“This is a civil rights bill, this is reparations, whatever you want to call it,” Limbaugh told his listeners in 2009.
Democratic lawmakers, meanwhile, deliberately linked their healthcare fight to past struggles for racial equity.
Before the critical March 2010 vote on the law, Georgia Rep. John Lewis, a civil rights icon who had participated in the famous 1965 march across the Edmund Pettus Bridge in Selma, Ala., when marchers were beaten by police, walked arm-in-arm with other lawmakers to the Capitol to pass the bill.
Adding to the historical echoes that day, several black lawmakers reported hearing racial epithets as they walked through the crowd of protesters outside the Capitol, many from the then nascent tea party movement. One lawmaker was spit on.
“It was like going into a time machine with John Lewis,” Rep. Andre Carson, a black Democrat from Indiana, observed at the time.
A decade later, some of that vitriol has faded. And the health gains made possible by the law have been striking.

Between 2013 and 2015, the share of African Americans without health insurance dropped by nearly half, falling from almost 25% to less than 14%, according to data assembled by the nonprofit Commonwealth Fund.
At the same time, African Americans reported skipping care less frequently because of concerns about cost, almost cutting the gap between blacks and whites in half.
And new research shows that inequalities in how quickly white and black patients start treatment for advanced cancers almost disappeared in states that fully expanded coverage through the health law.
“The law dramatically lessened disparities by race,” said Dr. Otis Brawley, an oncologist at Johns Hopkins University and former chief medical officer at the American Cancer Society.
In Arkansas, which was the first Southern state to expand Medicaid coverage through the law — Louisiana and Virginia have since followed — the impact has been particularly large.
The share of poor residents without health insurance tumbled from nearly 42% to just 19% between 2013 and 2014, researchers found.
The coverage gains allowed clinics like the ones in West Memphis and Marianna to expand services such as dentistry and behavioral health. They added more nurses, more case managers, more health educators and others to help the neediest patients.
Patients, in turn, are more frequently getting checkups and filling their prescriptions more regularly.

“What we’ve experienced in the last few years has been nothing short of amazing,” said Terrence Aikens, who led efforts at the West Memphis clinic to enroll patients in health insurance through the 2010 health law.
And yet, even now, as the Affordable Care Act enters its second decade, the gains feel tenuous to many here. The law’s opponents — including Arkansas’ governor and the Trump administration — are working to get the Supreme Court to overturn it.
“It is such a difficult history, and we have come so far,” said Ward-Jones, the director of the West Memphis clinic. “Sometimes, though, it feels like we take two steps forward and one step back.”
More to Read
Get the L.A. Times Politics newsletter
Deeply reported insights into legislation, politics and policy from Sacramento, Washington and beyond. In your inbox three times per week.
You may occasionally receive promotional content from the Los Angeles Times.











