Opinion: The decline in American life expectancy harms more than our health

- Share via
American life expectancy started dropping even before the pandemic. It’s a critical barometer of our nation’s health and a sign that all is not well in the U.S.
Much of the increase in preventable, premature death is attributable to drug overdose, which increased five-fold over the last couple decades. But this malaise is far broader, driven largely by growing chronic illness.
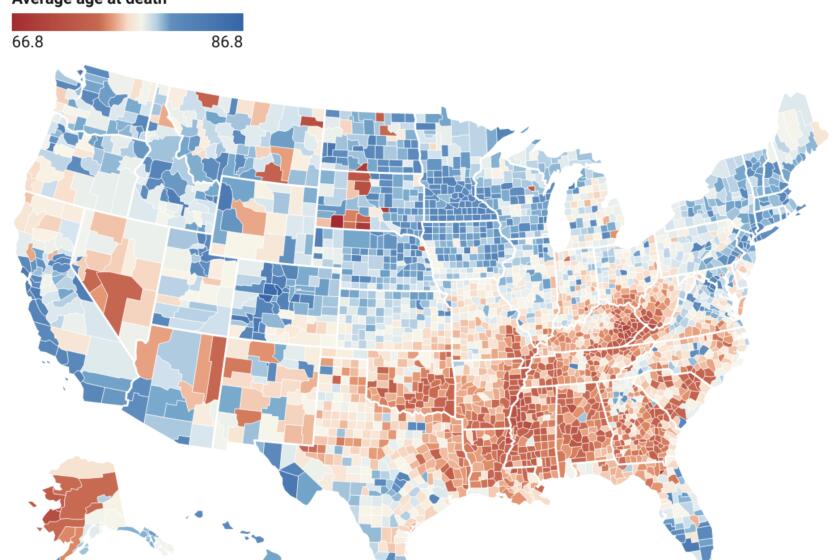
After decades of increasing longevity, Americans are facing shorter life spans than their predecessors and their rich-country peers. In states where Republicans set the agenda, it’s even worse.
Rates of depression are reaching new highs. Obesity rates among adults have risen from 30% to 42% since the turn of the century, with severe obesity nearly doubling and driving up the risk of cardiovascular disease, diabetes and other serious health conditions. The return of vaccine-preventable illnesses has been a concern since the 2010s. Sexually transmitted infections have surged in the last decade. And for the first time since 1937, an infectious disease, COVID-19, became one of the top three causes of death in the country.
These health problems are alarming on their own. They also have a devastating impact on our economy. A one-year increase in life expectancy could boost economic output by 4%. On the other hand, as Americans’ health declines, our health expenditures continue to soar. As a country, we spend $4.5 trillion annually on health, representing 17% of GDP. Out-of-pocket healthcare costs have risen dramatically, straining workers’ finances and pushing people into bankruptcy. All this fuels a cycle of a sicker workforce and a weaker economy.
Policymakers acknowledged the link between the economy and public health at the height of the pandemic, providing federal relief programs such as cash assistance and paid sick leave designed to keep the nation’s workforce and economy as healthy as possible. But our abandonment of these efforts since getting COVID relatively under control sets our country up for mounting crises. We need to revive a historical source of support for public health measures: the business case for a healthy workforce.
State laws to roll back public health powers during outbreaks of deadly disease contradict U.S. history.
In 1842, Edwin Chadwick argued in his landmark “Report on the Sanitary Conditions of the Labouring Population of Great Britian” that public health investments are crucial not only from a moral perspective, but also for economic productivity. Writing for the Atlantic in 1909, C.-E. A. Winslow, an American public health pioneer, wrote that employers who try welfare measures for workers “find that it pays.” And around that time, Wickliffe Rose, an American philanthropist, oversaw the Rockefeller Sanitary Commission to tackle hookworm disease as a controllable health problem, spurring economic productivity.
Hookworm, which can cause anemia and fatigue and impair development in children, was a significant problem in southern states in the late 1800s and early 1900s resulting from lack of access to clean water, poor sanitation and poor hygiene. Its symptoms were blamed on “laziness” — a stigma often attached today to symptoms of chronic illnesses, disabilities and mental health issues — and perpetuated cycles of poverty. Rose all-but-eradicated hookworm through education campaigns, expanding access to treatment and improving public sanitation.
Similarly, during World War II, the U.S. government invested in public health initiatives to curb the transmission of malaria in tropical and subtropical battlefronts; vaccinate against smallpox, typhoid fever and tetanus; and control sexually transmitted infections, which during World War I cost the U.S. Army more than 7 million workdays and 10,000 preventable discharges.
‘Rather than thinking of 75 as the time to die,’ let’s reimagine a world in which it’s a ‘robust time of engagement and work.’
When it functions well, such public health infrastructure makes it easier for working people to lead healthy lives. The results have been dramatic, contributing in the last century to the average human lifespan doubling around the world.
Despite the impression given by COVID-19, public health has historically been about so much more than tracking disease outbreaks. It’s been about preventing disease. Access to healthcare and insurance play a role, but doctors and hospitals most often come into play after someone is already sick. Research shows that simple resources such as clean air and water, affordable healthy food, stable housing and safe workplaces are much better predictors of good health and longevity.
During the pandemic, programs addressing basic needs — eviction freezes, expanded food assistance and mandated paid sick and family leave for employees in smaller companies — enhanced housing stability, curbed COVID spread and protected Americans’ mental health. Since then, home affordability has plummeted; half of American renters spend more than 30% of their income on rent and utilities. In 2022, more than 40 million Americans lived in food-insecure households, adding to health issues in adults and children.
Californians’ average life expectancy fell by two years due to COVID and drug overdoses, according to the Centers for Disease Control and Prevention.
The U.S. is one of the only high-income nations that still lacks universal paid sick leave and family medical leave, forcing many people to go to work sick or risk losing a day’s wages. Interventions to improve workplace air quality, a vital component of a healthy workplace appreciated even by 19th and 20th century health reformers, have been overlooked.
The pandemic-era measures were dropped in part because of their cost. But what is much more expensive, and what is causing American workers needless suffering as our national health declines, is our current approach to health. Of our $4.5-trillion annual health spending in the U.S., the vast majority goes to treating people when they are already sick; only 4% supports programs to keep people and workers healthy in the first place. This focus on treating individuals after they have already fallen ill is much of the reason we pay dramatically more than other countries yet still have some of the worst health indicators in the world.
Once again treating public health as an economic imperative could help broaden support for the type of interventions that became polarizing during the pandemic — but have a long track record of improving wellbeing and productivity.
Céline Gounder (@CelineGounder), an infectious-disease physician and epidemiologist, is the senior fellow and editor-at-large for public health at KFF Health News. She is also the host of the podcast “Epidemic.” Craig Spencer (@Craig_A_Spencer) is an emergency medicine physician and professor of public health at Brown University.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.