Procedures often result in risky preterm births
- Share via
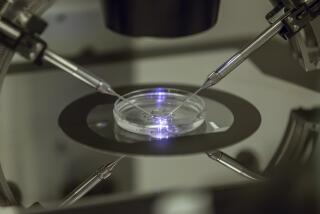
While the U.S. fertility industry has created thousands of families over the last 25 years, its successes have been shadowed by an alarming rise in multiple gestations and a corresponding increase in high-risk preterm births.
The problem is a consequence of both scientific advances and economic realities in an expensive and risk-driven field.
On one hand, improvements in laboratory techniques and clinical methods have boosted pregnancy rates and led to greater demand for fertility procedures. But as success rates have climbed, doctors and patients have been slow to abandon the practice of transferring multiple embryos in the hope that at least one will take.
Often, more than one does. In 2003, a third of all births generated by assisted reproduction produced more than one infant, 10 times the rate for the general population, according to the U.S. Centers for Disease Control and Prevention. Three percent of those births were of triplets or more, accounting for nearly half of all higher-order multiple births in the country.
The impact on premature births and other pregnancy complications is unsettling. Sixty-four percent of twins conceived through assisted reproduction and 97% of higher-order multiples are born preterm, defined as less than 37 weeks’ gestation, according to the CDC. Similar proportions are born with low birth weights.
In addition, mothers carrying multiples are more likely to have gestational diabetes, high blood pressure, preeclampsia and anemia, and to deliver by caesarean section.
Recent research also has found that even singletons conceived by in vitro fertilization are twice as likely to be born preterm as those conceived naturally. Scientists have yet to determine whether that might be due to underlying fertility problems, the age of women who typically use IVF, or the mechanics of assisted reproduction itself.
“People need to understand the downside as well as the upside of these technologies,” said Dr. Richard E. Behrman, chairman of a committee that recently examined the surge in preterm births for the National Academies Institute of Medicine.
The panel’s report said the rapid growth of assisted reproduction in the U.S. has contributed to a 30% increase in the preterm birthrate over the last 25 years.
The infant mortality rate for children born between 32 and 36 weeks of gestation is nearly four times the rate for full-term babies, according to the CDC. For babies born before 32 weeks, the mortality rate is 75 times higher.
Those who survive are sometimes afflicted with lifelong disabilities. The institute’s report conservatively estimated the annual economic burden of caring for preterm children at $26.2 billion, or $51,600 per child.
“It’s a major priority on our radar screen,” said Dr. William E. Gibbons, president of the Society for Assisted Reproductive Technology.
That group’s parent organization, the American Society for Reproductive Medicine, first attacked the problem in 1998 by adopting voluntary guidelines aimed at curbing the number of embryos transferred in assisted reproduction procedures. In 2004, it toughened those guidelines, recommending for women under 35 that doctors transfer no more than two embryos “in the absence of extraordinary circumstances” and only one “for patients with the most favorable prognosis.”
It is too early to measure the effects, but some progress had been noted even before the guidelines were published. The rate of higher-order multiples dropped 120% from 1996 to 2003, according to the CDC, though the rate of twinning in assisted reproduction stayed virtually static.
The fertility industry is largely unregulated in the U.S. But a number of countries, primarily European, have enacted laws restricting the number of embryos that doctors can transfer. Other countries have built incentives for singleton births into their national health plans.
Gibbons said his group is revising its guidelines again, focusing this time on reducing transfers of the 5-day-old embryos known as blastocysts. Some studies suggest that blastocysts implant at a slightly higher rate than the more commonly used 3-day-old embryos.
Fertility specialists have an economic incentive to transfer multiple embryos because consumers often pick doctors based on their pregnancy success rates.
Patients, meanwhile, typically spend tens of thousands of dollars on fertility treatments, often without insurance coverage. As a result, they may be focused on doing whatever it takes to get pregnant. And given the cost of replicating the process, some patients simply angle for twins.
The result: In 2003, more than half of all transfers were of three or more embryos, and only 8% were of a single embryo, according to the CDC.
Some research suggests that for many women, the transfer of a single high-quality embryo may be just as likely to produce a pregnancy as the transfer of two or more. But that notion has yet to take hold in fertility clinics. To encourage doctors to regulate themselves, the Institute of Medicine report recommended that success rates be redefined to reflect not just pregnancies but singleton births.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.