Mattresses and mold removal: Medi-Cal to offer unconventional treatments to asthma patients
- Share via
MADERA, Calif. — Growing up amid the dusty agricultural fields of the Central Valley, Ruby Marentes-Cabrera can’t recall a time when it wasn’t difficult to breathe.
Diagnosed with asthma early in childhood, the ninth-grader has come to detest the pistachio trees that surround her home because the dust, pesticides and other allergens that blow off the orchards often trigger an asthma attack — even infiltrating her home so that simple chores like vacuuming can be dangerous.
“We live so close to the fields — I breathe the dust and chemicals in,” said Ruby, 14, describing coughing and wheezing fits calmed by puffs from her emergency inhaler or breathing treatments from a nebulizer. “It gets so bad that my back hurts, my head hurts, my lungs hurt. I get sick and it gets really hard to breathe.”
Ruby is among roughly 2 million low-income Californians who have health insurance coverage from Medi-Cal, the state’s Medicaid program, and have been diagnosed with asthma, a chronic and expensive disease that costs California billions of dollars per year in healthcare spending, missed work for parents and lost school days for kids.
The disease — exacerbated by air pollution and indoor threats like harsh cleaning products, cockroach infestations, dust and mold — hits low-income communities the hardest. Medi-Cal patients accounted for half the state’s asthma-related emergency and urgent care visits in 2016, even though they represented about one-third of the population, according to data cited by state health officials.
Starting in January, California will embark on an ambitious experiment to control asthma in its most vulnerable patients. Medi-Cal will offer recipients like Ruby unconventional in-home “treatments” not traditionally considered healthcare: removing mold, installing air purifiers and even replacing carpeting, blinds and mattresses.
These new asthma benefits are just a small part of Gov. Gavin Newsom’s sweeping $6 billion initiative to transform the largest Medicaid program in the country. The initiative, known as CalAIM, will target the state’s sickest and most expensive patients and cover an array of new social services, including home-delivered healthy meals; help with grocery shopping, laundry and money management; and security deposits for homeless people in search of housing.
Newsom’s goal is to lower soaring Medi-Cal spending — which hit an astronomical $124 billion this fiscal year — by preventing costly care such as emergency room visits. But state health officials acknowledge the new asthma benefits may not actually save taxpayer money.
Nor will the benefits be distributed equally: Because Medi-Cal managed-care insurance plans have immense power to decide which new services to offer and to whom, the initiative will create a patchwork of haves and have-nots. Of the 25 participating insurance companies, 11 will offer in-home asthma services starting in January in 36 of the state’s 58 counties. Within those counties, some Medi-Cal recipients will qualify; others will not.
“It’s a mystery,” says one expert. Some 2 million Californians were projected to join Medi-Cal, the state’s insurance program for low-income people.
With just two weeks to go before the program debuts, many insurers are scrambling to establish networks of nonprofit organizations and private contractors that specialize in delivering in-home asthma services and home repairs.
In San Bernardino and Riverside counties, for example, about 400 patients served by the Inland Empire Health Plan — out of nearly 1.4 million Medi-Cal plan members — will have access to asthma services in the first year, largely because the insurer has identified only one organization equipped to handle the responsibility.
“If we don’t do this right, this dream can become a nightmare,” said Alexander Fajardo, executive director of El Sol Neighborhood Educational Center in San Bernardino, which is negotiating a contract with the insurer.
Fajardo said El Sol is frantically preparing. While his organization has experience providing asthma education, it doesn’t have expertise in medical billing, patient privacy regulations and managed-care contracts.
“This is new, so we still have to learn,” Fajardo said.
Jeanna Kendrick, the Inland Empire Health Plan’s senior director of care integration, called the experiment to develop new social services “probably the hardest thing we’ve ever done.” It pushes plans into uncharted territory, she said, contracting with community organizations and teaching them how to handle medical billing, for example.
“We really do need to be creative and have some wiggle room because this is brand new for all of us,” Kendrick said.
Jacey Cooper, California’s Medicaid director, argued earlier this year that health plans will start small but add capacity over the five years of the initiative. The state is offering incentive payments to help plans launch new services and has set aside $300 million for the first half of 2022 alone.
The Department of Health Care Services, which administers Medi-Cal, could not say how many low-income Californians will receive new in-home asthma services, because they are voluntary, and as a result could not predict future costs. But Anthony Cava, a department spokesperson, cited data showing that more than 220,000 Medi-Cal recipients have poorly controlled asthma. The state pays $200 to $350 for a typical asthma-related emergency room visit, and $2,000 to $4,000 a day for a typical inpatient hospitalization, department officials said.
Agency officials couldn’t confirm the asthma benefits will save money, saying the costs will be equal to or less than the costs of traditional medical treatments.
Under the program, health insurers will send contractors into houses and apartments to assess hazards and educate patients about conditions that can trigger asthma attacks. Insurance executives say they will consider approving any service that could help asthma patients — from replacing tattered carpets to buying nontoxic cleaning products and pillow dust covers — within the $7,500 lifetime cap for each Medi-Cal recipient. The services will be available to both renters and homeowners.
“It’s not that somebody can just say they just want a brand-new $3,000 mattress,” said Dr. Takashi Wada, chief medical officer for the Inland Empire Health Plan. “But we do think a lot of these asthma attacks are preventable, and by avoiding illness, you’re also avoiding unnecessary hospital and emergency department visits.”
Fresno and Madera counties have some of the worst air quality in the state. They also have the highest rates of childhood asthma-related ER visits in California, along with Imperial County on the Mexican border, according to 2019 state public health data.
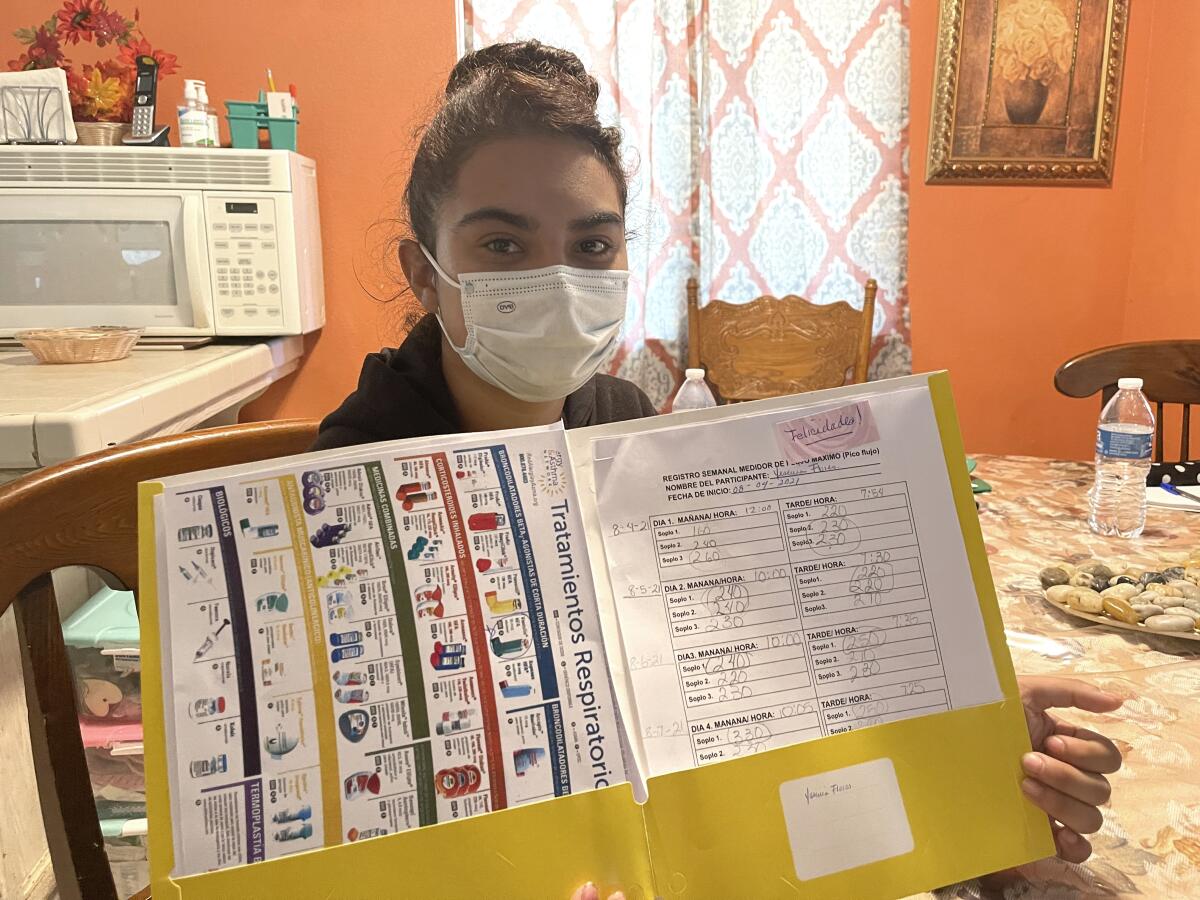
Ruby and her family, who live in Madera, Calif., appear to be ideal candidates for state-funded asthma benefits, said Joel Ervice, associate director of Regional Asthma Management and Prevention, which lobbied for the new services. Both Ruby and her sister Yesenia, 20, have asthma and were frequent visitors to the ER during childhood.
But as in the Inland Empire, only a small share of Central Valley asthma patients will receive the new services initially. Ruby and her family hope they will be among the lucky ones but realize they may still have to rely on conventional treatments such as emergency inhalers — and the hospital if necessary.

“I’m taking my medication a lot right now — it would be good if my asthma got better,” said Ruby, who wants to be able to play outside her home and excel in outdoor school activities. “I’m having a hard time running the mile in school, so being able to run would be so great for me and my health.”
CalViva Health, a major insurer serving patients in the Central Valley, including the Marentes-Cabrera family, so far has identified one nonprofit organization to deliver services and is negotiating with others.
That organization, the Central California Asthma Collaborative, expects to be able to serve up to 500 people across seven counties next year. Unlike other nonprofit groups that are still assessing how to deliver services, the collaborative has already identified private contractors to remove mold, install bathroom or kitchen ventilation, and provide other services, co-director Kevin Hamilton said.
CalViva Health CEO Jeffrey Nkansah said asthma is one of the leading causes of hospitalization among the insurer’s enrollees.
“But right now, these conversations around identifying partners to deliver these asthma remediation services are fluid,” Nkansah said. “We’re still working hard to make sure we can get those services in place for Jan. 1.”
For the Marentes-Cabreras, the relentless clouds of dust and other toxins from orchards, combined with seasonal wildfire smoke, are the biggest problem. The particles infiltrate their lungs and their home, covering surfaces and caking the carpet, which they would like to replace. But they don’t have the money.
For now, Sandra Cabrera uses nontoxic cleaning products, and daughters Ruby and Yesenia track their lung capacity with oxygen meters.
“I am trying to control what’s in the house to prevent them from getting sick, cleaning a lot and using different cleaners,” Cabrera said in Spanish. “We could use help to do more, but it’s really difficult.”
KHN (Kaiser Health News) is one of the three major operating programs at KFF (Kaiser Family Foundation).
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.










