Column: Nurses know we were unprepared for the coronavirus. They’re being punished for speaking out

- Share via
When Chelsea Halmy reported for her nighttime shift in the COVID-19 unit at Providence St. John’s Health Center in Santa Monica on April 11, she made what she thought was a routine request: to be provided with an N95 respirator mask before coming into contact with patients.
As she knew, the N95 masks were the most effective in the hospital’s stock for blocking potential infection by the novel coronavirus that causes the disease. Her supervisor said no; standard surgical masks were good enough, she was told.
When Halmy refused to treat patients without the N95 equipment, she was brought into a closed room where a supervisor, reading from a script that Halmy captured with her smartphone, threatened her with a charge of insubordination and a report to the state Board of Registered Nursing for “patient abandonment,” which could result in the loss of her nursing license.
We started asking employers back in January how they were preparing for the potential pandemic. We saw right away that they weren’t prepared.
— Bonnie Castillo, National Nurses United
Per Halmy’s telling, the supervisor named a COVID-19 patient. “Will you accept a direct order to accept assignment” of the patient? “Yes or no?”
“I said, ‘Yes, I want to accept my assignment,’” Halmy told me. “’However, I don’t feel safe going in the room without an N95 respirator.’” Asked again, she repeated the answer.
Three fellow nurses told me they were subjected to the same treatment that night, as seven others had been earlier in the week. All were sent home.
As of Friday, the 10 nurses who demanded N95 protection before working in the COVID-19 unit were still suspended, even though the hospital has backed off from its insistence that N95 masks aren’t necessary for nurses in the unit.
Having received new supplies as well as government approval to reprocess N95 masks, the hospital says, it is now able to “provide them to all caregivers treating COVID-19 patients.”
The hospital refused to comment on the status of the suspended employees. The California Nurses Assn., which represents the nurses, says that seven of the nurses had had “investigative” meetings with managers by Friday but had been sent home afterward without a resolution of their cases.
The post-coronavirus reopening is up to consumers, not Trump or governors.
Workers in many front-line occupations requiring direct contact with the public, such as grocery workers, can be dangerously exposed to the novel coronavirus.
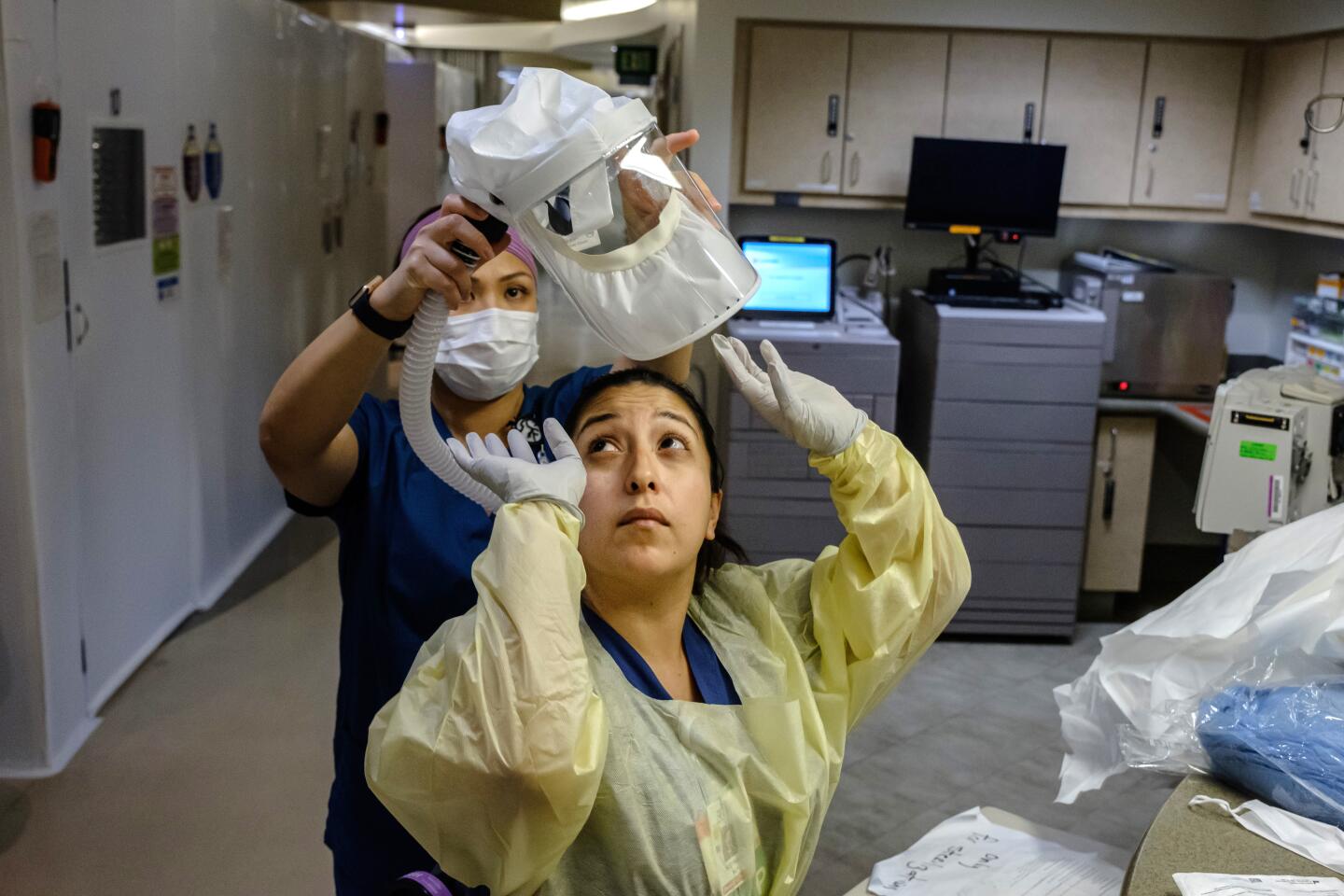
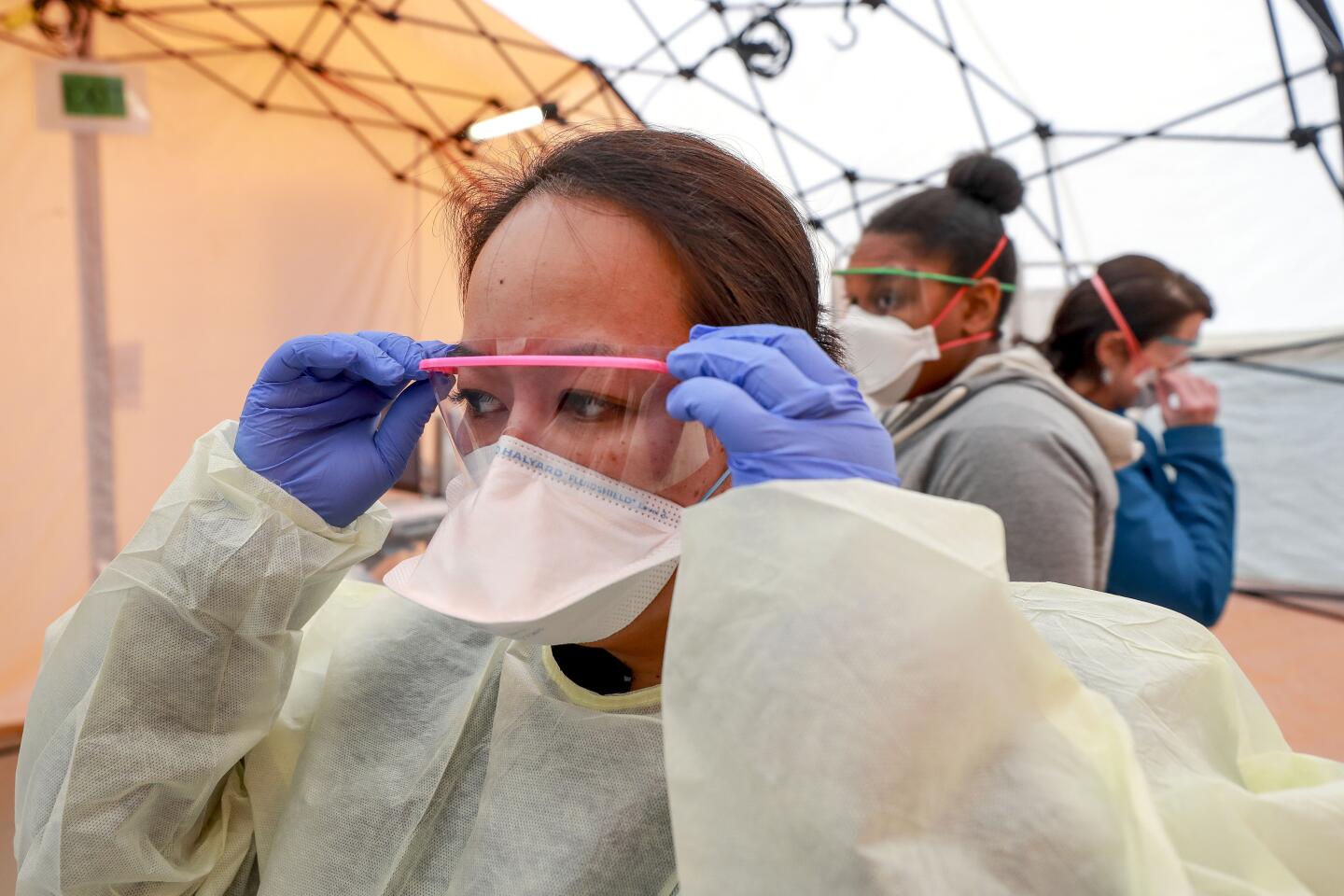
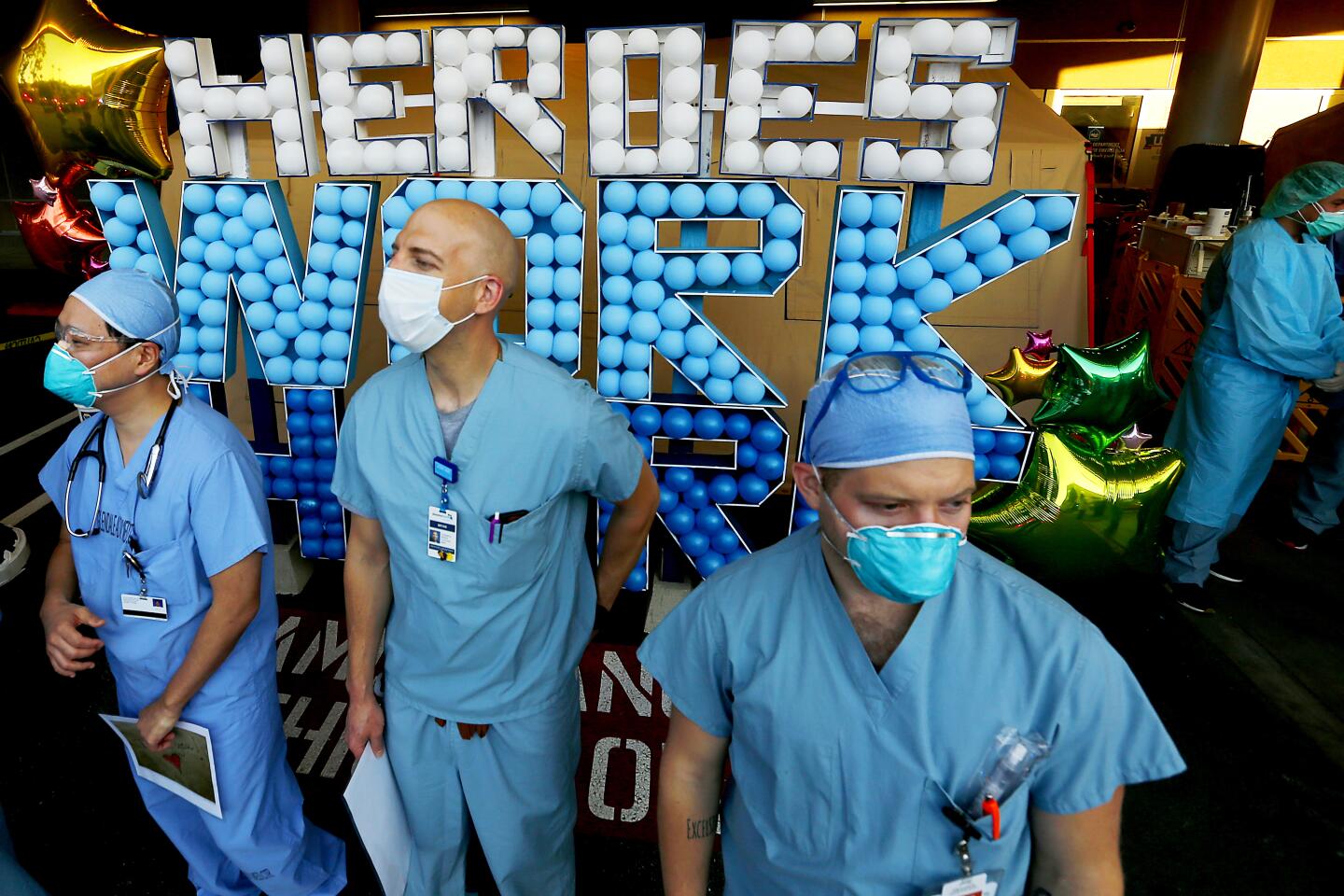
But healthcare workers may be the most vulnerable. Their work requires them to come into closer contact with COVID-19 patients and in more confined spaces than other workers. Nurses particularly spend more time with patients than most other hospital employees and therefore may have a better sense of their institutions’ level of preparedness for disease outbreaks than their professional colleagues.
As my colleagues Anita Chabria, Harriet Ryan and Soumya Karlamangla report, the coronavirus has taken a significant toll on healthcare workers in California, with more than 175 cases at UCLA and at least eight cases at Providence St. John’s.
As of Thursday, according to National Nurses United, the parent of the California union, 320 members have tested positive for COVID-19 nationwide, and 40 nurses have died of the disease.
During the coronavirus outbreak, as it happens, nurses seem to have suffered an outbreak of management threats of discipline and terminations. These have occurred in connection with nurses’ insistence on being provided with the highest-grade personal protective equipment, or PPE, or with public critiques of their institutions’ operational shortcomings.
“Nurses aren’t afraid of caring for COVID patients,” says Malinda Markowitz, president of the California nurses union. “But nurses are the only professionals who are at the patients’ bedside 24/7. They’re worried about themselves and about passing the infection on to their families or other patients. But the hospitals feel that RNs are expendable.”
Some nurses have faced discipline for bringing PPE from home or raising money to buy it for their colleagues. Kaiser Permanente, the giant national managed care organization in Oakland, threatened to fire nurses “on the spot” if they were caught using their own N95 masks, according to the nurses union.
Medical experts are not finding much to like in Trump’s chloroquine treatment.
“Kaiser is insisting that this is not an airborne disease, that it only needs droplet protection, and therefore you only need a surgical mask,” says Diane McClure, a registered nurse at Kaiser’s South Sacramento location and a union official. “But there’s a lot about the disease that’s not known, and we want the highest-level protection first.”
After the Kaiser nurses made the management threat public, Kaiser management issued an email telling staff that they wouldn’t be disciplined for wearing their own masks, the union says. A Kaiser spokesman told me by email: “We are not and have not been disciplining nurses or other staff for bringing in their own protective equipment.”
Other nurses and some physicians have also been disciplined for posting public complaints about the lack of preparedness at their hospitals. Jhonna Porter, a supervising nurse in the COVID-19 ward at HCA Healthcare’s West Hills Hospital, was suspended on March 23 after she posted an alert to a private nurses’ Facebook group about inadequate supplies and asked for community donations for herself and colleagues in her unit.
HCA says Porter was suspended for posting “specific information, including room numbers of possible COVID patients,” to Facebook, which it implied was a violation of patient privacy laws. Porter was reinstated on April 8 after an investigation established that the violation was “inadvertent,” HCA said.
Porter says that she posted no patient information and that HCA was citing the Health Insurance Portability and Accountability Act “to save face.” Her suspension sent an intimidating message to employees to prevent them from speaking out. “They didn’t shut me up,” she told me, “but they shut a lot of other people up.”
She says West Hills, where the COVID patient count more than doubled to 25 in the weeks she was suspended, is still doling out N95 masks to staff piecemeal, sometimes using donated supplies. HCA, the largest for-profit hospital chain in the country, earned $4.1 billion on revenue of $51.3 billion last year.
Hospitals may be cracking down on nurses and other whistleblowing professionals out of embarrassment.
Without minimizing the scale of the economic plunge, it’s proper to place comparisons between today’s figures and economic situation and those of the Depression in perspective. In short: The differences are greater than the similarities.
“A lot of hospitals were caught off-guard” by the coronavirus pandemic, says Blake Horwitz, an attorney representing Lauri Mazurkiewicz, a nurse who was fired in March by Northwestern Memorial Hospital in Chicago after she emailed 50 fellow nurses with a warning that N95 masks offered better protection than the masks the hospital had distributed to the nursing staff.
“They’ve employed the knee-jerk response of not wanting to be caught with their pants down,” Horwitz told me. The professionals, however, “are speaking out on a matter of public concern. These are straight-out retaliation cases.”
Hospital managements should keep in mind that nurses don’t take lightly to being pushed around. They’re outspoken, organized, knowledgeable and adept at presenting their case in terms of patient protection.
In 2005, then-Gov. Arnold Schwarzenegger learned that to his misfortune when he attempted to delay a tightening of staffing-to-patient ratios in California hospitals and denigrating them as a special interest. The nurses launched a public campaign against the change and eventually secured a court ruling upholding the tighter standards.
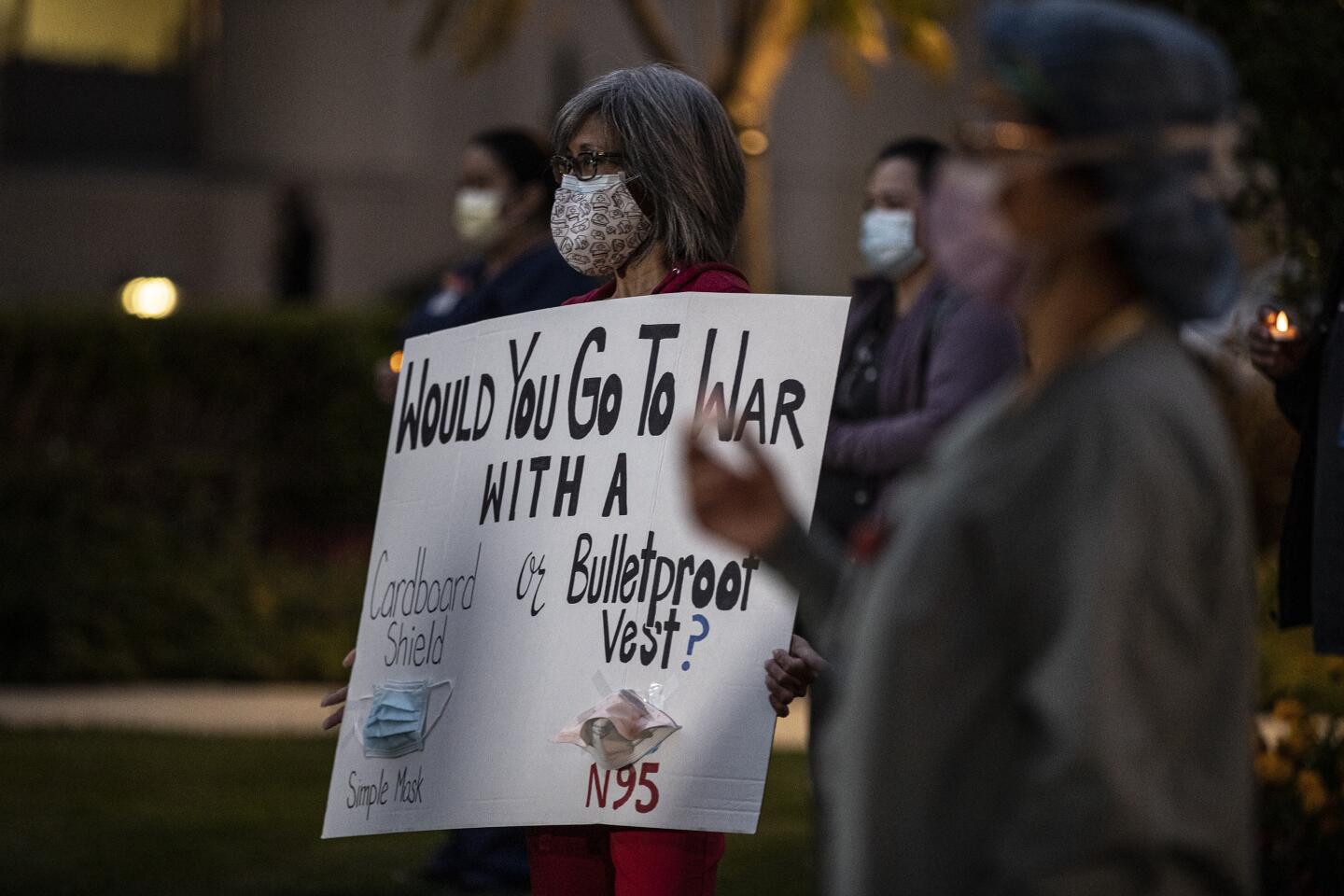
In the current crisis, supplies of N95 masks — so designated because they’re designed to filter 95% of airborne particles — are in such demand that authorities say they should be reserved for front-line healthcare workers.
The coronavirus crisis has stopped Trump’s attack on Medicaid in its tracks
The very fact that this equipment needs to be rationed is a scandalous commentary on American public health preparedness.
“We started asking employers back in January how they were preparing for the potential pandemic,” says Bonnie Castillo, executive director of the California Nurses Assn. and its parent, National Nurses United. “We saw right away that they weren’t prepared, mainly because they subscribed to just-in-time stocking of supplies and equipment, similar to how they staff in general. But when we demanded PPE, we were met with discipline.”
The cases at St. John’s illustrate Castillo’s point. The suspensions began the morning of April 9, when several nurses arrived at the first-floor unit reserved for patients who had tested positive for COVID-19 or were awaiting test results. They were issued paper masks.
“A couple of staff physicians coming onto the unit to do their patient rounds were wearing hospital-issued N95 masks,” says Michael Gulick, one of the nurses. “When they saw us, they were bewildered why we weren’t wearing N95 masks. The doctors said we’re taking care of an unknown disease and the hospital should be using the most conservative safety protocol.”
Supervisors refused to issue the masks. Gulick says that when he stood his ground, he was taken into a private room and subjected to the same scripted interrogation that Halmy described.
But the issue that confronted Halmy and her colleagues wasn’t scarcity; she and other nurses say their supervisors never claimed that the supply of N95 masks at St. John’s was so short that the masks needed to be conserved. Rather, the practice was based on protocols set down by the Centers for Disease Control and Prevention.
The hospital says that at all times, every nurse caring for COVID-19 patients or those awaiting test results was provided with “appropriate” protective equipment according to guidelines issued by the CDC, the World Health Organization and the state.
The CDC’s guidelines state that flimsier surgical masks are good enough for healthcare workers unless they’re working with patients in extremely close quarters. The CDC placed this advice, however, in the context of “crisis capacity strategies,” including the reuse of equipment that was designed for one-time only use or that had exceeded its manufacturer-designated shelf life. The CDC acknowledges that these steps could “pose a risk of transmission between [healthcare personnel] and patients.”
Those words are a reminder that it’s not only nurses who are punished when hospital managements retaliate against them for whistleblowing. Patients are too. Nurses know how to recognize preparedness, and when they find it wanting they should be heeded, not punished.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.