Global Warning
While science foresees major advances in the next millennium in treating cancer and heart problems, genetic disease and even mental illness, infectious diseases--the No. 1 killers worldwide and No. 3 in the United States--remain a major sticking point within the so-called Biological Revolution.
Within the next five to 10 years, no crucial advances are in sight with the potential to slow expansion of the global epidemics of HIV, drug-resistant tuberculosis, or malaria, scientists say.
âWeâre on the verge of the 21st century with all this modern technology,â says Larry Gostin, a professor of law at Georgetown University and expert on AIDS and human rights, âand yet weâre as vulnerable to pathogens as we were decades ago.â
Perhaps the best example of this is acquired immune deficiency syndrome. As the numbers of AIDS cases and deaths in America continue their sharp decline since 1994, itâs tempting to view the epidemicâs future optimistically. But experts interviewed earlier this year outlined a disturbing two-tiered future in which, lacking a vaccine, the disease continues to grow at an alarming rate among the poor in both the United States and throughout the world, exacting huge tolls on society in most Third World countries.
This gloom may come as a surprise to those familiar with recent HIV treatment developments involving combinations of three or more antiviral drugs. Called HAART, for highly active anti-retroviral therapy, the treatment has revolutionized HIV care since being introduced in summer 1996.
But as the 21st century dawns, experts say that HAART is clearly not the answer for all: Its price tag alone--$10,000 to $60,000 a year for the drugs--renders the therapy inaccessible for more than 90% of the worldâs HIV-infected population, now estimated by the United Nations AIDS Programme at 33.4 million people.
Even in North America and Western Europe, where hundreds of thousands are currently on HAART, trouble is brewing. Many--about 50%, depending on which studies are cited--fail their initial rounds of therapy because they canât tolerate its toxic side effects or adhere to its rigorous daily dosage schedules. And missed doses promote emergence of drug-resistant viruses, allowing the human immunodeficiency virus infections to swell and sicken the individual.
Finally, there is a realization that what was initially whispered about as a possible cure is now seen as no more than another difficult palliative, a treatment that keeps symptoms at armâs length. In 1997 and 1998, studies found evidence of vast, hidden reservoirs of HIV in successfully treated patients that experts now say will still plague the patients 25 to 30 years down the road.
Worse yet, it now appears that these reservoired viruses continue to reproduce and even mutate, despite seemingly effective HIV treatment.
âThereâs ongoing replication and cell-to-cell infection even in the presence of HAART,â explains Dr. Mario Stevenson of the University of Massachusetts in Amherst. âSo it may not be [HIV] latency. It may be continued viral production. And how that occurs in the face of effective drugs is a mystery. All we know is the pattern: continued low-level replication and virus evolution.â
Time Still Major Enemy for People With HIV
Dr. Emilio Emini, of the Merck Research Laboratories in West Point, Pa., says time remains the major enemy of people with HIV.
âThere are patients who, even though theyâve suppressed virus for years, will fail,â Emini says. âSo what does that tell you? It tells you itâs not an easy consideration to, quote-unquote, cure a patient. Even after a long time of suppression . . . the virus will cycle up.â
So is there a solution? Experts hold out little hope of a final cure, differing significantly in their outlook only on one point: How many decades will pass before an effective, affordable vaccine is developed for use worldwide?
âWeâve said from the beginning this is a nasty little virus,â Emini says. âMy fundamental hope is that in the end weâll be able to make a sincere shot at a vaccine here.â
The National Institutes of Health also have reached the conclusion that a vaccine is the only thing that can slow HIVâs seemingly relentless expansion. Currently, half the agencyâs $1.8-billion HIV budget is aimed at the search for a vaccine, says Neal Nathanson, director of the Office of AIDS Research.
âWeâre in it for the long haul,â he says. But he argues that the private sector lacks similar long-term commitment to the problem: âNone of the big players [the worldâs large pharmaceutical firms] are seriously involved in developing a vaccine at this time,â he says. âThey donât see the profit in it.â
At Glaxo Wellcome, the worldâs largest multinational pharmaceutical company and a major player in HIV drug development, Peter Young, the vice president for HIV therapeutics, only shrugs: âI think weâre probably as far away from treatment cures as we are from vaccines.â
One problem is that each time the virus population cycles up, that means itâs managed to mutate to resist one or more of the HAART drugs. Doctors then must change the patientâs combination, drawing from a list of more than 250 drug triads currently licensed in the United States. But most mutations confer HIV resistance not only to just one individual drug, but also to that entire class of drugs.
So each new HAART combination lasts for less time than its predecessor, and eventually patients run out of treatment options as their highly resistant viruses overwhelm the body, explains Dr. Michael Saag of the University of Alabama.
âSo now weâve evolved from a cure paradigm back to a palliative care one,â Saag says. âPerhaps the biggest difference . . . is we now should expect failure with whatever [combination] we first use.â
With the bloom clearly off the HAART rose, AIDS advocates are calling for rapid development of drugs that hit novel targets on HIV, possibly outwitting the virusâ awesome mutation capacities. But Emini says there isnât much in the drug development pipeline, and itâs impossible to answer when such novel agents might be ready.
âWhere will we be in 10, 20 years?â asks Dr. Peter Piot, the director of UNAIDS, the United Nationsâ program on HIV-AIDS. âItâs really, really hard to say. We havenât done [forecasts] going out more than to 2005. Weâve learned that the projections turn out to be awfully wrong.â
Indiaâs Huge Number of Cases Affects Forecast
For more than a decade, epidemiologist Jim Chin executed HIV forecasts for the World Health Organization and UNAIDS. Now retired and living in California, he believes that there will continue to be from 25 million to 30 million people with HIV alive each year for the next 25 years.
By then, he says, âhopefully, the African countries can get their act together and begin significantly reducing their annual incidence of new infections so that 50 years from now . . . the global prevalence will begin to drop to about 10 to 20 million--with well over 95% in developing countries and the vast majority [80% or more] in Africa.â
Grim as that scenario may be, Chin concedes that India, with a population of nearly 1 billion people, is the âwild cardâ that could throw off the forecasts.
A recent joint publication of the World Health Organization, Harvard School of Public Health and the World Bank, titled âHealth Dimensions of Sex and Reproduction,â predicted that much of Africa wouldnât see its HIV epidemic peak until 2005 to 2010. Asiaâs epidemics, the paper said, wouldnât peak until a decade later.
If true, and if an adult infection rate higher than 30% indeed constitutes societyâs HIV bell peak, the world could have nearly half a billion people living with HIV and AIDS by the year 2020.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, says it is figures like these that have prompted his agency to target half of its HIV spending toward vaccine development.
Fauci is more optimistic than many experts that an acceptable vaccine will soon be developed.
âWe may not get a perfect vaccine within a decade,â he says. âBut Iâll bet you a Sicilian pizza that we have some form of moderately effective vaccine [against disease progression] within a decade.â
Ancient Diseases Account for Half of All Deaths
But AIDS is not the only problem faced by medical experts dealing with infectious disease. The helplessness felt in the face of HIV is mirrored in battles against a host of bacterial and parasitic diseases, many of which are either not treatable or, for a variety of reasons, are not being properly treated. And so ancient scourges, such as malaria and scarlet fever, continue to account for nearly half of the world populationâs annual deaths. Dr. Bernard Pecoul, of the humanitarian organization Doctors Without Borders, is convinced that a key solution is lowering the cost of essential drugs for poor countries.
If the worldâs top pharmaceutical companies follow their current cost trajectories, âthey will end up only focused on the 300 to 400 million people in the richest countries,â he says. âWe cannot accept that, for most of the world, the essential drug list is now things from the 1950s and â60s, many of which cause drug resistance.â
Whatâs at stake? A time bomb, Pecoul warns, of resurging infectious disease--strengthened by drug resistance--that will explode not just in the worldâs poorest countries, but in Europe and America as well. The global village will be affected, he says.
Indeed, a forecast by researchers at UC San Francisco predicts that by 2070, the world will have exhausted all antimicrobial drug options, as the viruses, bacteria, parasites and fungi evolve complete resistance to the human pharmaceutic arsenal. It is a vision that remarkably is shared by many of the worldâs top microbiologists and infectious diseases experts.
âPeople are looking at new targets for antimicrobials,â Dr. Stanley Falknow of Stanford University says. âBut itâs not clear they will work.â
Although several laboratories are working on novel ways to kill bacteria and viruses, Falknow says, no fundamentally new approaches are expected to be available within the next 10 years. And if such drugs do reach the marketplace they will undoubtedly follow the financial pattern set with antibiotics: Each newer drug costs far more than its predecessor. And the newer agents are usually more toxic, their use fraught with fiercer side effects.
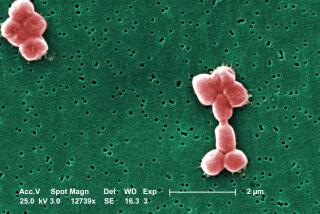
The biggest concern is staphylococcus, for which only one drug is left, Falknow says. If that were incurable it would be devastating, because the bacteria, which cause a wide range of life-threatening diseases, are highly contagious.
Fauci warns that mutated microbes resistant to hosts of drugs are the real crises looming for the 21st century.
The drug companies, meanwhile, are banking on vaccines. They say innovative products, such as vaccines made from the DNA of viruses or bacteria, will be available for tuberculosis, malaria, the diarrheal disease schistosomiasis and other killers within 20 years. And, they say, these vaccines will be affordable.
But Dr. Phillip Lee, former second-in-command at the U.S. Department of Health and Human Services, says heâs heard that before.
âHere we are, 100 years after Pasteur identified the cause of rabies and [Robert] Koch the cause of tuberculosis,â Lee says. âYet we did more to control TB by social factorsâ than by any vaccine, and today more people globally die of tuberculosis than in Kochâs day.
âOne hundred years out,â he says, âand we still donât have a vaccine for tuberculosis or malaria.â