FDA Revisits Forbidden Ground
A biotechnology company working on a new AIDS vaccine wants to be able to test it on volunteers.
Another company has a new influenza vaccine that can be quickly manufactured in the face of a fast-moving sudden epidemic.
But neither firm can proceed in the U.S. because these new vaccines are grown in âneoplasticâ cells--cancer cells or cells that cause tumors when injected into animals--and their use is prohibited.
That may be about to change. The Food and Drug Administration is considering ending a 45-year-old ban on using such cells to produce vaccines.
The prohibition, a matter of practice rather than law, was based on the fear that viruses and genetic material hidden in the cells could contaminate a vaccine, exposing recipients to the risk of cancer or other diseases that might not show up for years after immunization. The issue is of particular concern because most vaccines are given to children.
Vaccine developers say that growing vaccines in the prohibited cells offers several advantages over the standard methods: faster production in response to deadly disease outbreaks; reduced costs to consumers; and fewer surprises, like unexpected viruses that have sometimes popped up in standard vaccines.
And for certain viral diseases, like AIDS, these cells may provide the only way of producing an effective vaccine.
The agency âis being asked to move beyond the precedent that was established back in 1954 against the use of cell lines established from tumors,â Dr. Andrew Lewis, head of the FDAâs DNA Virus Laboratory, told members of the agencyâs vaccine advisory committee at the first public discussion of the issue late last year.
Dr. Sidney Wolfe, director of the Public Citizens Health Research Group and a frequent critic of the FDA, worries that the agency could be pressured by the industry into ending the moratorium before it has done a careful, independent job of reviewing the production methods needed to be sure a vaccine is safe.
âThe reason for a 45-year moratorium on human or animal tumor cells is the concern about material from the tumor . . . that could be activated in a vaccine,â Wolfe said. Using the forbidden cell types âis an unknown. It has not been done, and if you do it, you have to be very careful.â
Those advocating the change say the cells--which continue to divide indefinitely--have been studied for years and that there are now methods to test for and remove any contaminants from vaccines grown in them.
âIn my opinion, arguments against human tumor cells are crazy,â said Ronald C. Desrosiers, a Harvard Medical School researcher, who has been working on a live AIDS vaccine that has been licensed to Therion Biologics. Concern about contamination with cancer-causing viruses âwas a realistic fear 20 or 30 years ago,â he said, but not any longer.
Desrosiers and Therion Biologics have been developing an experimental AIDS vaccine, one that contains a live but defective version of the human immunodeficiency virus that causes the disease. The genetically manipulated virus is grown on tumor cells taken from a human lymphoma.
The human immunodeficiency virus âgrows only in human cell lines, not in other types of cells,â said Margaret Johnston, assistant director of AIDS vaccines at the National Institutes of Health, at the FDAâs vaccines advisory committee meeting in November.
Although Therion has no immediate plans for human trials, the company has approached the FDA about what it would have to do to test the vaccine, said the companyâs president, Dennis Panicali.
âThe FDA acknowledges that the risk is very remote and that there may be ways to virtually eliminate it,â Panicali said.
A Dutch company, Solvay Duphar, has completed tests of a new influenza vaccine in Europe--a killed virus grown in cells that cause tumors when injected in mice. Company officials have talked to the FDA about the use of the cells, derived from dog kidneys, in producing a vaccine for use here. To date, no vaccine produced in these cells has been approved in the U.S.
The mammalian cells offer several advantages over fertilized chicken eggs, which can be in short supply in the face of a major flu epidemic.
To conduct its tests, the company convinced regulators in several European countries of the safety of its product, said Bram Palache, who managed the clinical trials of the new vaccine. âThe flexibility in production will be a breakthrough in technology,â he said.
But the canine cells cause tumors in certain laboratory mice, and the FDA has not allowed them to be used in vaccine production in the U.S. Palache said his company has talked to the FDA about testing the new flu vaccine in the United States but has no immediate plans to do so.
Montreal-based Biochem Pharma Inc. is also testing a flu vaccine grown in canine kidney cells, but Claude Vezeau, president of the companyâs vaccine subsidiary, says researchers have been able to modify the cells so they no longer cause tumors in the mice.
In the U.S., the company has joined forces with SmithKline Beecham and hopes to begin trials here by early next year.
Vezeau says the safety of any vaccine cannot be predicted with 100% certainty. âYou can take a flight tomorrow, and although flights are very safe, once in a while one crashes,â he said. âYou want to be able to measure the risk.â
*
The FDA plans to convene its vaccine advisory panel again this summer to discuss the issue of using the new cell lines.
Before moving ahead, the agency âhas to be convinced that safety is being met,â the FDAâs Lewis told committee members. Until the FDA reconsiders the ban, no company will be allowed to test such a vaccine in volunteers.
Some believe the FDAâs decision will require a careful weighing of benefits of a new vaccine versus the potential risks.
âThe risks will never be nothing. We all know that,â the NIHâs Johnston said.
Many scientists believe there are a number of steps vaccine manufacturers can take to reduce or eliminate the risks of using tumor cells. But even the required testing in large numbers of volunteers will not necessarily turn up all the problems caused by a new vaccine.
âThereâs concern about a rare event, something that occurs in less than one in 50,000,â said Dr. Brian Murphy of the laboratory of infectious diseases at the National Institute of Allergies and Infectious Diseases. âYouâd never see it until the product goes into widespread use.â
And physicians worry about taking any step that might undermine confidence in vaccine safety in the minds of an already wary public.
âThe public today is a very different public than it was [45 years ago] ago when polio vaccine came on the market and the response was: âDoes it work? Here, give it to me,â â said Dr. Theodore Eickhoff, a professor of infectious diseases at the University of Colorado Health Sciences Center. âThe public for a whole variety of reasons has become much more distrustful of the vaccine enterprise. . . . And when they hear about vaccines produced in neoplastic [cancer] cells, that will set some peopleâs teeth on edge.â
At the heart of the controversy is the way vaccines, which are made from killed or weakened viruses, are grown.
Unlike most living things, viruses cannot reproduce by themselves. They are the biological equivalent of an instruction manual, equipped with all the information needed to build copies of themselves but few of the tools. In order to grow, they must invade living organisms, where they commandeer the machinery of their hostâs cells. And each virus is highly particular--it will only grow in specific cells in selected species.
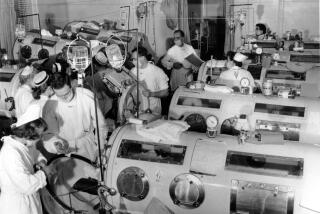
The prohibition against using tumor and other abnormal cells for vaccines began in 1954 when the U.S. Army was considering the best way to produce a new vaccine for a serious respiratory infection that often strikes recruits in boot camp. The military doctors decided not to risk using tumor cells, long used in research laboratories.
The earliest vaccines were live or killed viruses, grown in whole animals or fertilized chicken eggs and then separated from the cells that spawned them. But chicken eggs from certified, disease-free flocks are sometimes in short supply.
Manufacturers have turned to animal and human cells grown in the laboratory. Chicken cells, for example, are now routinely used to produce measles and mumps vaccines. Polio vaccines are grown in monkey kidney cells.
There were problems with some of the early vaccines. A number of people working with the monkey cells that were used to grow the first polio vaccines, for example, died from monkey-borne viral infections.
And from 1955 to 1963, polio vaccines were later found to be contaminated with another monkey virus, SV40, which caused cancer in rodents. Numerous studies have turned up no connection between the defective vaccine and development of cancer in those who were vaccinated.
Today, however, all vaccines are routinely checked for contamination from stray viruses and any remaining cell fragments.
In the 1970s, after a decade of contentious debate, the agency approved the first vaccines grown in human âdiploid cellsâ--laboratory-grown cells derived from the lungs of human fetuses that can divide 50 times or more. Master stocks of these cells can be frozen, stored and then thawed whenever needed to grow the large number of cells needed for vaccine production.
These cells, which do not cause tumors when injected into animals, are now used routinely in measles, hepatitis A and rabies vaccines.
In the 1980s, the FDA permitted the use of tumor-causing cells to produce genetically engineered proteins for the treatment of cancer, heart disease and other disorders.
Winning approval for the first genetically engineered product made in tumor cells wasnât easy, recalled Jack Obijeski, who was director of vaccine development at Genentech Inc. in South San Francisco.
Genentech scientists had found a way to produce a new clot-busting drug in cells taken from Chinese hamster ovaries. Before it could win approval to test the purified protein in patients, it had to show that the product was not contaminated with cell material or viruses that might cause cancer in humans.
âEveryone was afraid of the unknown,â Obijeski recalled. âWe did experiment after experiment.â
The drug, called Activase, won FDA approval in 1987 and is widely used in emergency rooms to treat heart attacks. It is one of at least 18 of these proteins now on the market--including interferon and the anti-anemia drug Epogen.
*
Times staff writer Paul Jacobs can be reached via e-mail at [email protected].