Computer-Aided Therapy Used to Curtail Guesswork of Drugs
- Share via
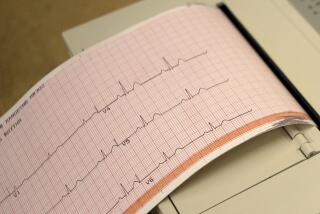
A heart attack victim is receiving the first of a long series of injections of the powerful cardiac drug lidocaine to treat an abnormal cardiac rhythm.
For such a critically ill patient, so-called miracle drugs can make the difference between life and death. So powerful are these medications, even minor deviations in therapy can prevent--or cause--major complications.
In the past, during the earliest moments of critical care, the physician has had very little data about just how the patient’s body is functioning, leaving little more than subjective clinical judgment to make important life-and-death decisions.
But at a number of medical centers nationwide computers are revolutionizing medicine by eliminating prescription guesswork and quickly achieving optimal therapy for critically ill patients.
Dr. Roger W. Jelliffe, a clinical pharmacologist and cardiologist at USC, is among a handful of researchers who have pioneered the field of computer-assisted drug therapy. During the last 20 years he has been painstakingly transcribing the rules of drug behavior onto computer software.
Originally, it took a mainframe computer to house all the pertinent information; today, his software will run on small personal computer and is operating at 30 institutions.
His goal, he said, is to develop computer programs that can be packaged on floppy disks and distributed to the medical community in much the same way that business programs, such as spreadsheets and data bases, are distributed to other professionals.
This will create “a powerful new medical tool,” Jelliffe predicted, one that will “revolutionize patient therapy” and allow for optimal patient care “whether the patient is in a small rural hospital or a giant urban medical center.”
The key to this technology is a series of complex mathematical models based on how certain drugs behave in different bodies, he explained. These models can be used to predict how a drug will behave in a particular patient.
“Each patient’s (drug) therapy is an inevitable experiment, because each patient is different,” Jelliffe said. “These (mathematical) models at least allow you to start by applying what you know about people in general and people like this patient in particular.”
For example, by knowing a patient’s age, weight and cardiac function, it is possible to calculate how fast a drug such as lidocaine will be distributed throughout the body, the speed at which it will be used up or metabolized, and the rate at which the drug will either be broken down or excreted.
Close to Being Toxic
To be clinically effective, Jelliffe noted, some drugs must be administered in dosages that produce blood levels which are very close to being toxic.
For example, powerful antibiotics are often used to treat patients particularly vulnerable to infection, such as individuals who are severely burned or those whose immune systems are impaired. But if drug concentrations exceed therapeutic levels by even a small amount, the auditory nerve and kidneys may be damaged.
Powerful cardiac drugs, like digitalis and lidocaine, can save patients who are having or are at risk of having a heart attack. Or, at serum levels only slightly higher than necessary, they can induce life-threatening cardiac arrhythmias.
Complicating an already difficult situation is the fact that different bodies handle drugs differently. As Dr. Agneta Hurst, a clinical pharmacist who teaches at the USC School of Pharmacy, describes it, “A big 45-year-old construction worker is going to require a much different dosage than a 75-year-old lady who lives in a nursing home.”
Added Hurst: “Unfortunately, most of our current concepts about (drug) dosing are generalized and when you start looking at individual patients, they’re often not responding at all the way you would expect them to.”
Not Always Possible
Applying mathematical models can help, Jelliffe noted, but calculating such information at bedside isn’t always possible. Even with such calculations, a drug might also require a “step process,” which would mean administering a dozen or more doses at staggered intervals.
Even the best medical mind can’t manage all of these variables like a properly programmed computer can, said Jelliffe. “Physicians have to rely on subjective clinical judgment in order to estimate (drug) dosage. It’s a trial-and-error approach. But a computer can eliminate a large part of the guesswork.”
A computer can “learn” rapidly how the drug behaves in that patient, Jelliffe said. As treatment is administered, the patient’s response is measured and described. With each added bit of information, the computer model better reflects each patient.
Using the physician’s clinical goals and the patient’s vital statistics, the software calculates the dosages necessary to maintain the prescribed blood levels of the drug.
‘Smart Pumps’
So-called “smart pumps” can then be used to administer the drugs directly into the patient. Researchers at St. Jude Children’s Research Hospital in Memphis, Tenn., are already using smart pumps to administer chemotherapy and intravenous feeding. Other facilities are using smart pumps to administer analgesics for pain control.
The concept of a smart pump has been around for about 10 years, but, according to the developer of the USC smart pump, Dr. William Nicholson, now a fellow in cardiology at Stanford University, the earlier versions were bulky, complicated to use, and not so smart.
The computer--actually a hand-held programmable calculator--issues instructions to a pump, which controls the flow rate from an intravenous (i.v.) unit. Several days worth of an individual drug can be stored in the i.v. unit and administered without further assistance from nurses or hospital personnel.
“We have microwave ovens and videocassette recorders that are all programmed to start and stop at certain times and we take this for granted,” noted Jelliffe. “There is no reason why we can’t do this with infusion apparatus . . . rather than having a human being handling this onerous chore.”
If the rate of drug infusion needs to be changed, a few keyboard strokes are all that’s necessary.
Although these computerized systems are ideally suited for managing the critically ill patients within an intensive-care unit, Nicholson noted, “the applicability of this technology is immense.” He predicts it will eventually be used “in emergency rooms, in regular hospital wards, in the field by paramedics,” and perhaps, one day, even in the home.
But in the clinical setting, will physicians accept a floppy-disk partner? Will they feel like they have been demoted to taking samples and inputting data?
Doctors or Engineers?
“I think doctors are often the last people who want to use computers,” Jelliffe conceded with a laugh. “If they had wanted to be engineers, they wouldn’t have gone into medicine.
“Some (physicians) will probably resent these systems for one reason or another, but I think many clinicians will jump at the chance of having this kind of tool.”
The programs, he noted, are designed for people who have had “minimal or no training” in the use of computers. There is no programming necessary; the clinician simply responds to the prompts as the program takes him or her through the procedures necessary to individualize drug therapy.
The programs were designed for doctors, pharmacists and nurses. “They presume a background in drug therapy and management,” he said, “but they do not presume any computer literacy outside being able to hit the ‘Y’ key for Yes and the ‘N’ key for No.”
Safety features have also been built into the system to handle everything from typing errors to a dangerously aggressive drug regimen.
For example, if an unusually high blood level of a drug is requested, the computer provides data concerning adverse reactions associated with that level.
At the present time, only a few drugs are amenable to such management techniques. However, in the near future, Jelliffe believes a wide variety of pharmaceuticals, such as anti-cancer drugs, will lend themselves to such care.
“The computer will provide an objective means for improving both the theory and practice of medicine,” said Jelliffe. “It will help us better document our record of treatment--to see exactly how well we are doing and show us specifically how to improve.”