Two vaccines might get emergency approval this month. Hereâs what you need to know

By most assessments, the speed at which COVID-19 vaccines have been developed is remarkable.
Vaccines often take years to roll out, but the U.S. Food and Drug Administration, which is tasked with vetting and approving new medical products, released guidelines this summer that included a provision to authorize their emergency use. Such authorization would circumvent the typical protocols and allow a new vaccine to be distributed if âthe known and potential benefits of a product ⌠outweigh the known and potential risks.â
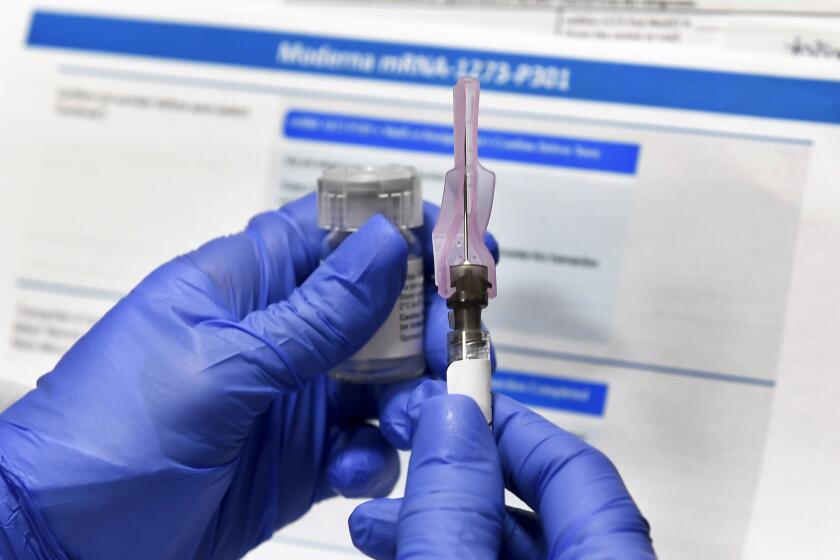
On Nov. 20, Pfizer and its partner BioNTech were the first to file for an emergency use authorization for their COVID-19 vaccine. On Monday, Moderna submitted its candidate for similar authorization. Both requests are under review.
The Pfizer and Moderna vaccines are both RNA-based vaccines and require two doses. The Pfizer vaccine doses need to be administered three weeks apart; the Moderna doses, four weeks apart.
A green light from the FDA could set into motion a rapid sequence of bureaucratic procedures and logistical steps that would result in the initial delivery of 6.4 million doses of the Pfizer vaccine throughout the United States and eight territories no later than Dec. 14. The company says it expects to produce up to 50 million doses by the end of the year.
The Moderna vaccine, if authorized, would be ready for distribution a week later. The company expects to have approximately 20 million doses available in the U.S. by the end of 2020.
âFar and away, this is the most ambitious vaccine program ever attempted, period,â said Dr. Kelly Moore, associate director of the Immunization Action Coalition, a nonprofit that provides information about vaccines and their distribution. Moore, a former member of the Centers for Disease Control and Preventionâs Advisory Committee on Immunization Practices, currently serves on an external advisory board for Pfizerâs coronavirus vaccine.
Where do we stand today?
In submitting their requests for an emergency use authorization to the FDA, Pfizer and Moderna forwarded data collected from clinical trials that had been conducted through November. An advisory committee with the federal agency â the Vaccines and Related Biological Products Advisory Committee â is reviewing the information.
Even though the results of the Pfizer trials have not been published in a peer-reviewed medical journal, the FDAâs investigation is âfar more detailed and rigorous than a peer review,â Moore said.
In addition, early results of Phase 3 trials for both vaccines have been vetted by an independent data and safety monitoring board.
When people talk about COVID-19 vaccines, they can sound like theyâre speaking a foreign language. Donât worry! Hereâs your guide to vaccine vocabulary.
When will we learn the FDAâs decision?
The advisory committee meets Dec. 10 to consider Pfizerâs request. Moore expects a decision to be made within a day or two, and if the FDA grants emergency use authorization, the vaccine could be on its way to medical centers throughout the U.S. no later than Dec. 14.
Moderna expects the committee to consider its request Dec. 17. If approved, its vaccine will be available as early as Dec. 21, StĂŠphane Bancel, the companyâs chief executive, told the New York Times.
Who will be eligible for the vaccine?
The Advisory Committee on Immunization Practices met Tuesday to debate and vote on who should be first in line to receive initial doses of a COVID-19 vaccine. They recommended that the initial vaccination effort focus on frontline healthcare workers, as well as residents of long-term care facilities, such as nursing homes and assisted-living facilities. As more vaccine becomes available, more groups will be eligible.
Their recommendations are nonbinding but âcarry great importance for public health and medical officials,â Moore said.
Tuesdayâs decision is intended to help states as they get ready to receive and distribute COVID-19 vaccines. The committee, however, will meet again to discuss and vote on specific vaccines once those vaccines have received FDA authorization.
As they gear up to execute the biggest vaccination program in U.S. history, officials know whatâs at stake, and theyâll face several major challenges.
What happens after the emergency use authorization is granted?
No vaccine doses can be shipped until the emergency use authorization has been granted, but the CDC and the federal Department of Health and Human Services have been working with states to determine where they will be delivered for what is known as âprepositioning,â Moore said. The goal of prepositioning is to identify locations where the vaccine can be delivered and administered once the emergency use authorization is granted.
At that point, states can place their orders for the vaccine through the CDC tracking system. The CDC will relay the information to the pharmaceutical companies, and shipments can begin.

How will the vaccines be shipped?
The Pfizer vaccine is being manufactured at the companyâs 1,300-acre facility in Kalamazoo, Mich. Shipments will be made from there and from a distribution center in Pleasant Prairie, Wis.
The nature of the Pfizer vaccine requires it to be kept at about minus 70 degrees Celsius. Pfizer has designed âtemperature-controlled thermal shippersâ with dry ice to maintain this frigid temperature. Once delivered, the vaccine will have to be stored in special freezers.
The vaccine will be shipped by FedEx or UPS in the special coolers, which are fitted with up to five trays. Each tray holds 975 doses, so each cooler can contain 4,875.
Because of the special requirements of the vaccine, the CDC recommends that it be shipped directly to where it will be administered to minimize handling. There will be an exception for rural parts of the country, where the targeted population is smaller than 975 and the doses have to be distributed more widely.
The Moderna vaccine is different. The company says its vaccine needs to be frozen, but only at minus 20 C, the temperature of a regular freezer. This requirement will make it easier for the vaccine to be stored in pharmacies or in rural areas that donât have ultra-cold freezers.
California and other states are racing to finalize plans for who will get the first doses of COVID-19 vaccines and how they will be delivered.
How will the initial vaccine shipments be allocated among the states and within California?
The number of doses each state receives will be based on its population, not the severity of the outbreak within its borders.
On Monday, Gov. Gavin Newsom announced that California is set to receive 327,000 doses of the Pfizer vaccine when the first 6.4 million doses are shipped. The state has not indicated how many doses of the Moderna vaccine it will initially receive.
California is developing its own guidelines for the prioritization and allocation of vaccine when supplies are limited, according to a spokesperson for the state Department of Public Health. The recommendations of the CDCâs Advisory Committee on Immunization Practices will be taken into consideration, the spokesperson said.
In Los Angeles County, the Department of Public Health is working with the state to determine the amount of vaccine each local hospital will receive. Once received, the vaccine can be administered to any of the early priority groups.
How will this play out in California?
On Oct. 27, the federal Department of Health and Human Services asked the state Department of Public Health to identify sites for prepositioning vaccine in California.
The state chose Cedars-Sinai Medical Center in Los Angeles, Mercy Medical Center in Redding, Rady Childrenâs Hospital in San Diego, UC Davis Health in Sacramento, UC San Francisco Medical Center, Valley Childrenâs Healthcare in Madera and Zuckerberg San Francisco General Hospital.
These medical centers were selected because they have âultra-low temperature freezers,â a large population of the âhighest riskâ healthcare workers and the ability to âredistribute vaccine outside their facility and network,â said a spokesperson for the state Department of Public Health. They will be used if prepositioning is required in the initial stage of the vaccineâs distribution.
If prepositioning is not required, other registered providers throughout the state will be able to receive and administer the vaccine. UCLA Health, for instance, has increased its cold-storage capabilities, according to a spokesperson, and will be able to assist the county or state if needed.
Distributing COVID-19 vaccine will be biggest health operation in L.A. history. Can the bureaucracy pull it off?
Will the stateâs safety review group slow down this process?
In October, Newsom announced an 11-member COVID-19 Scientific Safety Review Workgroup to assess the safety and effectiveness of any federally authorized COVID-19 vaccine. According to Dr. Art Reingold, the groupâs chairman, the committee has met twice and reviewed the publicly available data from the Phase 1 and Phase 2 clinical trials conducted by Pfizer.
Reingold does not anticipate the workgroupâs final assessment to delay the delivery and administration of the vaccines in California.
What happens next?
Once the vaccination process begins, states will receive periodic notices from the CDC about future allocations. The states will then decide where the vaccine is needed and where subsequent doses should be shipped.
What about those second doses?
The CDCâs vaccine tracking system will monitor who gets a first dose and will coordinate with Pfizer and Moderna on the shipment of the second doses. This means medical centers can administer all the doses they initially receive without having to hold onto half for the second shot.
How long before I can drive to my local pharmacy and get a vaccine?
If youâre healthy and a nonessential worker, you will have to wait. Most experts feel that the immunization effort in the United States will be in high gear by late spring and early summer of 2021, as Pfizer and Moderna continue to ramp up production, and other vaccine candidates complete their clinical trials and apply for emergency use authorization.
âThis is the first of anything like this,â said Dr. Rita Shane, chief pharmacy officer at Cedars-Sinai. âWeâre looking forward to seeing the world become a better place once this comes through.â
Until then, the coronavirus will continue to be a threat to public health. Masks and social distancing will continue to be important safeguards against getting COVID-19.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.