No one knows how many patients are dying from superbug infections in California hospitals

As many as 9,000 Californians are believed to die each year from hospital infections.
Many thousands of Californians are dying every year from infections they caught while in hospitals. But youâd never know that from their death certificates.
Sharley McMullen of Manhattan Beach came down with a fever just hours after being wheeled out of a Torrance Memorial Medical Center operating room on May 4, 2014. A missionaryâs daughter who worked as a secretary at Cape Canaveral, Fla., at the height of the space race, McMullen, 72, was there for treatment of a bleeding stomach ulcer. Soon, though, she was fighting for her life.
On her medical chart, a doctor scribbled âCRKP,â an ominous abbreviation for one of the worldâs most lethal superbugs, underlining it three times.
Doctors tried antibiotic after antibiotic. But after five weeks in the hospital, mostly in intensive care and on morphine because of the pain, McMullen died.
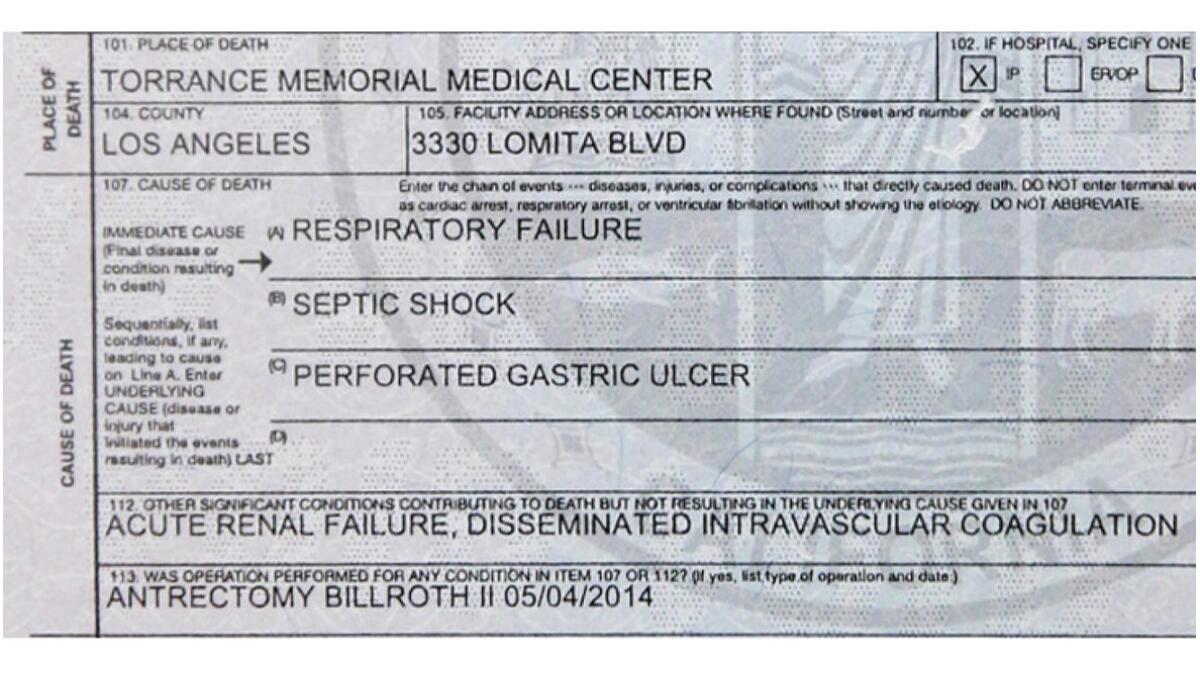
Her death certificate does not mention the hospital-acquired infection or CRKP, however. Instead, her doctor wrote that McMullen had died from respiratory failure and septic shock caused by her ulcer.
The doctorâs conclusion outraged Shawn Chen, McMullenâs daughter.
âIt should say she died of an infection she got in the hospital,â said Chen. âShe was so hardy. She would have made it through if it wasnât for this infection.â
Dr. Yasmeen Shaw, who treated McMullen in the ICU and filled out the death certificate, said she was following directions from health officials by recording the underlying cause of death, which in her opinion was the perforated ulcer.
âEverything that happened to her health is a consequence of the initial condition she came in with,â Shaw said. âHad the patient not have had a perforated ulcer they wouldnât have been in the hospital in the first place.â
An epidemic of hospital-acquired infections is going unreported, scientists have found.
University of Michigan researchers reported in a 2014 study that infections â both those acquired inside and outside hospitals â would replace heart disease and cancer as the leading causes of death in hospitals if the count was performed by looking at patientsâ medical billing records, which show what they were being treated for, rather than death certificates.
âEven if one person dies from a hospital-acquired infection, itâs one too many,â said Dr. Chesley Richards, who oversees the Centers for Disease Control and Preventionâs Center for Health Statistics and who met recently with a group of families to discuss the misleading death certificates.
California does not track deaths from hospital-acquired infections. And unlike two dozen other states, California does not require hospitals to report when patients are sickened by the rare, lethal superbug that afflicted McMullen, raising questions about whether health officials are doing enough to stop its spread.
McMullenâs daughter Chen said she called the Los Angeles County public health department to report that her mother had been diagnosed with CRKP, which stands for carbapenem-resistant Klebsiella pneumoniae, at Torrance Memorial. When the bacteria gets into a patientâs blood, it kills as many as half its victims.
A county employee told her it was not a reportable infection. âShe said, âItâs everywhere,ââ Chen said.
Torrance Memorial declined to answer questions about the accuracy of the death certificate or other questions about McMullenâs care. In a statement, the hospital said it âtakes patient safety, particularly as it relates to infection control, very seriously.â
Experts say hospitals can prevent the deaths through better infection control procedures, including some as simple as making sure staff wash their hands, but have little incentive to do so if the deaths are not reported.
âWe, the community of physicians, had been watching these patients die and trundling them off to the morgue for years,â said Dr. Barry Farr, former president of the Society for Healthcare Epidemiology of America, who is now retired. âNow weâre in the eighth verse of the same song.â
Federal health officials call CRKP and other species of pathogens in the broader family known as carbapenem-resistant enterobacteriaceae, or CRE, one of the nationâs most urgent health threats.
Because of the danger, the CDC recommends that local health officials require hospitals to report CRE cases. And if thatâs not possible, according to agency guidelines, health departments should still survey hospitals and nursing homes for the presence of the superbug to make sure facilities are trying to halt its transmission.
Chen said that at first the nurses at Torrance Memorial had taken extra precautions to keep the bacteria raging through her motherâs body from spreading by wearing disposable gowns and posting a sign on the door warning others from entering.
But Chen said she was stunned when her mother was moved to another floor where no such precautions were taken. âThere was a bedpan of urine sitting on a chair,â Chen said.
Chen said she worries that other patients may have been infected.
Torrance Memorial declined to comment on Chenâs report of a gap in safety precautions.
County health officials explained that they had stopped requiring health facilities to report CRE infections in 2012 âdue to resource limitations,â though some hospitals voluntarily submit bacterial samples from patients diagnosed with the superbug.
Infection cases gathered between 2010 to 2012 showed that Los Angeles County was âa high-prevalence regionâ for the superbug, county officials said.
County officials said they were working to prevent the infections, including by sending public health nurses to hospitals to consult on potential outbreaks and proper infection controls. They said they had no record of a complaint about a CRE case at Torrance Memorial.
The CDC estimates that 75,000 Americans with hospital-acquired infections die during their hospitalizations each year. Since California provides between 10% and 12% of the nationâs hospital care, state officials used the agencyâs analysis to estimate that 7,500 to 9,000 Californians die each year from infections from hospital germs.
But these numbers may be underestimated, perhaps by a great degree, experts say.
âItâs fair to challenge that number,â the CDCâs Richards said of the estimate of 75,000 deaths.
Sepsis can cause death when an infection spreads to the blood, triggering an inflammatory response that damages the bodyâs organs and causes them to fail.
In March, the CDC estimated that the actual number of deaths from sepsis were as much as 140% higher than those recorded on death certificates, or as many as 381,000 deaths a year. According to another study, 37% of hospitalizations for sepsis were caused by infections caught in hospitals or other health facilities like nursing homes.
That suggests that as many as 140,000 Americans are dying each year from healthcare-acquired sepsis, just one subgroup of the infections.
McMullen came to Torrance Memorial for an elective hernia surgery in late April 2014. A week later, her husband rushed her to the emergency room because she was suffering from abdominal pain and weakness.
ER doctors suspected she was losing blood from a perforated ulcer in her stomach. Their suspicion was confirmed through two procedures with an endoscope. She had surgery to stop the bleeding on May 4. By the next day, doctors had diagnosed her infection and sepsis.
McMullenâs medical records, which her family provided to The Times, detail how doctors became frustrated as the drugs they prescribed â including colistin, known as the antibiotic of last resort â did not help. Soon McMullen was in critical condition.
The CDC advises hospitals that have a patient with CRE to test other patients nearby and those who have shared the same medical equipment to ensure others are not infected.
The Times asked Torrance Memorial officials whether any other patients were infected with CRE in 2014 or 2015 and if any of those cases may be linked to the bacteria that sickened McMullen. Officials declined to answer those questions.
We, the community of physicians, had been watching these patients die and trundling them off to the morgue for years.
— Dr. Barry Farr, former president, Society for Healthcare Epidemiology of America

Without mentioning McMullen, Torrance Memorial officials said that during 2014 the bacteria âseem to have contributed to the death of one patient, who likely acquired CRE while hospitalized.â
Yet they ruled out the endoscopes â the source of recent superbug outbreaks at three other Southern California hospitals â as the cause of McMullenâs infection. Officials said âfollowing an extensive investigationâ they had âdetermined that there have been no known cases of CRE transmission by endoscopeâ at the hospital.
One reason doctors are reluctant to report in public records that patients have died from hospital-acquired infections, experts say, is the possibility of malpractice lawsuits.
CDC officials warned in October that they had discovered that some hospitals had tried to stop their infection-control staff from reporting certain types of hospital-acquired infections to a national database as required.
In a 2010 survey published in a CDC medical journal, 49% of New York City medical residents said they had knowingly reported an inaccurate cause of death on a certificate.
Nile Moss, 15, unexpectedly died a couple days after having an MRI at Childrenâs Hospital of Orange County in Orange in 2006.
An autopsy showed that he died from a rare superbug, methicillin-resistant Staphylococcus aureus, or MRSA, which the CDC says is a leading cause of healthcare associated infections.
His parents say they believe the pad patients lay on in the MRI machine was contaminated with the bacteria. The teen was hit with flu-like symptoms soon after having the outpatient test. He was hospitalized after his fever reached 104 degrees and he struggled to breathe.
The doctor did not list the bacteria on Nileâs death certificate. Instead he wrote the teen had died from âadult respiratory distress syndrome.â Contributing causes, the doctor wrote, were septic shock and pneumonia.
âDoctors have the ability to write whatever they want,â said Nileâs mother, Carole Moss, one of the people who attended the CDC meeting on inaccurate death certificates. âMany people are angered by this. They cause the harm and then cover it up.â
Denise Almazan, a spokeswoman for the childrenâs hospital, said officials were looking into the teenâs case and could not immediately comment.
Ed Winter, assistant chief in Los Angeles Countyâs medical examiner-coronerâs office, said that any case in which a patient is suspected of dying from an infection acquired from hospital procedures should be sent to the medical examiner for review to determine whether county officials rather than hospital doctors should determine the cause of death.
âIf there is a question, we will look into it,â he said.
If the autopsy and facts of the case conclude a patient died from the infection, the death certificate would state âacquired infection after surgical procedure,â Winter said.
In May, Dr. Martin Makary, a surgeon at Johns Hopkins Hospital in Baltimore, called on the CDC to add a line to all death certificates where doctors would be asked if the death was caused by a preventable complication from medical care.
Makary estimates that infections, errors and other cases of âmedical care going wrongâ would be at least the third-leading cause of death among Americans if they were properly recorded.
âWe need an open and honest conversation about the problem,â Makary said.
Twitter: @melodypetersen
MORE BUSINESS NEWS
Bayer wonât fight EPA ban on pesticide
Donald Trump dumps on LAX, but L.A. Mayor Eric Garcetti defends airport upgrades
Volkswagen reaches $1.2 billion settlement with U.S. dealers over emissions scandal
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production â and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.











